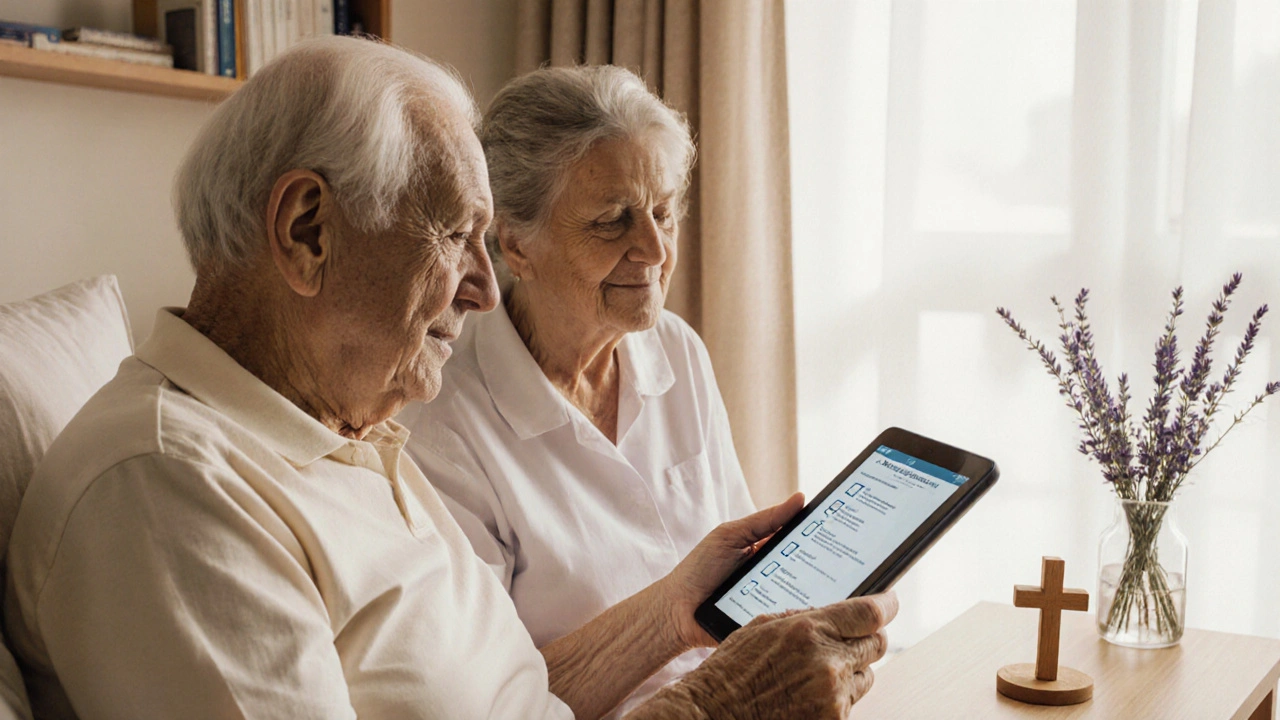
Spiritual Care Checklist for Dementia Patients
This checklist helps caregivers evaluate and implement spiritual care practices tailored to individuals with dementia. Check off items as they are completed.
- Ask about spiritual background during intake
- Record preferred rituals, music, or texts
- Identify a chaplain or spiritual liaison
- Schedule daily or weekly spiritual activities
- Provide sensory tools (music, scent, tactile objects)
- Monitor mood and behavior before and after activities
- Adjust practices based on observed response
- Document everything in the care plan
- Offer training for staff and family members
- Review the spiritual care plan quarterly
0 out of 10 items completed
Keep going! Spiritual care makes a real difference in the lives of those with dementia.
- Start with 2-3 activities that resonate with your loved one
- Keep sessions short (5-10 minutes) for consistency
- Use familiar music, scents, or objects to evoke comfort
- Encourage family involvement when possible
- Track changes in mood or behavior over time
Quick Takeaways
- Spirituality can lower agitation and improve mood for people living with dementia.
- Integrating faith‑based or secular practices fits naturally into person‑centered care plans.
- Start small: music, prayer, reminiscence, or nature walks are easy entry points.
- Train caregivers on cultural sensitivity and ethical boundaries.
- Use our checklist to make sure spiritual needs are routinely assessed.
When dealing with dementia, many focus on medication and safety, but Spirituality in Dementia Care is the practice of recognizing and supporting a person’s deeper sense of meaning, purpose, and connection, whether rooted in religion or personal belief can be a game‑changer. Below we break down why it matters, how to weave it into daily routines, and what tools are available for families and professional caregivers.
Understanding Spirituality and Dementia
Dementia is a progressive loss of cognitive functions such as memory, language, and reasoning, affecting roughly 55 million people worldwide. While the brain’s ability to process new information declines, parts of the emotional and spiritual brain often stay active longer than expected.
In parallel, Spirituality refers to the personal search for meaning, purpose, and connection to something larger than oneself, which can be expressed through religion, nature, art, or inner reflection. It isn’t limited to organized faith; it includes any practice that nurtures the soul.
When these two worlds meet, the result can be a calmer environment, stronger identity, and better overall wellbeing for the person with dementia.
Why Spirituality Matters in Dementia Care
Research from the 2023 International Journal of Geriatric Psychiatry found that participants who engaged in weekly spiritual activities showed a 30% reduction in agitation scores compared to those receiving standard care only. The same study noted higher scores on the Quality of Life‑AD (QoL‑AD) scale, especially in the “Emotional Well‑being” domain.
Key benefits include:
- Emotional grounding: Familiar prayers or hymns trigger long‑term memory pathways, offering comfort when short‑term memory fails.
- Identity preservation: Spiritual rituals reinforce a person’s sense of self, countering the loss of role that dementia can bring.
- Reduced behavioral symptoms: Calm breathing, meditation, or sacred music can lower cortisol levels, easing anxiety and aggression.
- Family cohesion: Shared spiritual moments create a bridge between caregivers and loved ones, improving communication.
From a Person‑centered care perspective, spirituality is a core dimension of the person, just like physical health or social interaction.

Practical Ways to Integrate Spiritual Care
Below is a step‑by‑step guide you can adapt to home settings, assisted living facilities, or hospice environments.
- Assess spiritual preferences early. During the initial care plan, ask open‑ended questions such as “What gives you a sense of peace?” or “Are there songs, prayers, or stories that are important to you?” Document answers in the care record.
- Build a resource list. Identify local chaplains, clergy, or interfaith volunteers. Many hospitals have a Chaplain service that can provide on‑call spiritual support.
- Incorporate daily rituals. This could be a 5‑minute prayer before breakfast, a short meditation session, or listening to a favorite hymn while getting dressed.
- Use sensory‑based spiritual tools. Aromatherapy with frankincense, soft lighting from a candle‑like LED, or a tactile prayer bead can engage multiple senses, reinforcing the spiritual experience.
- Leverage music therapy. Music therapy has been shown to trigger autobiographical memories; play songs from the person’s youth or religious choir recordings.
- Facilitate community connections. If the individual belongs to a faith community, arrange virtual or in‑person visits when possible. Even a short greeting from a familiar clergy member can be uplifting.
- Document outcomes. Track changes in mood, agitation, or sleep quality after each spiritual activity. Over time, you’ll see which practices have the biggest impact.
Remember, the goal isn’t to impose belief but to honor the person’s existing worldview.
Common Challenges and How to Overcome Them
Challenge 1: Unclear religious background. Some families may not know the person’s faith history.
Solution: Use a simple questionnaire that asks about favorite holidays, music, or rituals. Even a vague answer like “I liked being outdoors” can guide nature‑based spiritual activities.
Challenge 2: Caregiver discomfort with spiritual topics.
Solution: Provide brief training modules that focus on listening skills, cultural respect, and boundaries. Role‑playing scenarios helps staff feel confident.
Challenge 3: Institutional policies restricting religious items.
Solution: Work with administration to create a policy that allows personal spiritual objects (e.g., a small cross, prayer book) while respecting infection‑control standards.
Challenge 4: Fluctuating cognition. A person may be lucid one day and confused the next.
Solution: Keep spiritual activities simple and repeatable. Repeating a familiar hymn daily builds a sense of stability even when memory is spotty.
Resources for Caregivers and Families
- Books: “Spirituality and Dementia” (2022) - offers case studies and practice tips.
- Websites: The Alzheimer’s Association has a “Faith & Memory” toolkit with printable checklists.
- Organizations: National Hospice and Palliative Care Organization (NHPCO) runs an online chaplain training program.
- Apps: “Calm” and “Insight Timer” include guided meditations suitable for dementia patients.
- Local Support: Flagstaff Community Church runs a volunteer companionship program for seniors.
Checklist for Spiritual Support in Dementia Care
- Ask about spiritual background during intake.
- Record preferred rituals, music, or texts.
- Identify a chaplain or spiritual liaison.
- Schedule daily or weekly spiritual activities.
- Provide sensory tools (music, scent, tactile objects).
- Monitor mood and behavior before and after activities.
- Adjust practices based on observed response.
- Document everything in the care plan.
- Offer training for staff and family members.
- Review the spiritual care plan quarterly.

Frequently Asked Questions
Can spiritual care help reduce medication use?
Yes. Studies show that regular spiritual activities can lower the need for antipsychotic drugs by up to 15% in people with moderate‑to‑severe dementia, primarily because agitation and anxiety decrease.
What if the person has no religious affiliation?
Focus on secular spirituality: nature walks, art appreciation, “life story” storytelling, or mindfulness breathing. The goal is the same-connection and meaning.
How often should spiritual activities be scheduled?
Consistency matters more than length. A 10‑minute session once or twice a day works well for most residents. Adjust frequency based on observed mood changes.
Is it okay for non‑faithful staff to lead religious rituals?
Ideally, a trained chaplain or volunteer who shares the resident’s faith leads the ritual. If that’s not possible, staff can facilitate by playing recorded prayers or music while respecting personal boundaries.
What signs indicate that spiritual care is effective?
Look for reduced agitation, improved sleep, more smiles, increased eye contact, and positive verbal or non‑verbal cues during or after sessions. Tracking these signs weekly helps quantify benefit.
It is with a profound sense of gravitas that I observe the intersection of spirituality and dementia care, a realm where the intangible meets the clinical; indeed, the literature is replete with data, yet the human heart still seeks narrative. The checklist presented is commendable, but one must ponder the underlying epistemology that informs each item, for without theoretical rigor the praxis may become perfunctory. Moreover, the integration of sensory tools such as incense or tactile beads raises ethical considerations regarding consent, especially when cognitive capacity fluctuates. One cannot ignore the cultural heterogeneity of spiritual expression, thereby demanding that caregivers adopt a pluralistic lens, lest they inadvertently impose a monolithic worldview. The cited 2023 International Journal of Geriatric Psychiatry study, while robust, should be contextualized within a broader meta‑analysis to ascertain external validity. Practically speaking, scheduling daily rituals must be balanced against caregiver fatigue, a factor often under‑reported in implementation guides. The recommendation to document every encounter is laudable, yet the administrative burden may deter compliance, suggesting the need for streamlined digital tools. In terms of outcome measurement, mood scales and cortisol assays provide quantitative backing, but qualitative anecdotes remain indispensable. The emphasis on family involvement is wise, but boundaries must be delineated to protect both patient dignity and caregiver wellbeing. Finally, the periodic review of the spiritual care plan, as proposed, should incorporate multidisciplinary feedback, ensuring that chaplains, nurses, and occupational therapists align their efforts. In sum, the checklist is a valuable scaffold; however, its efficacy will ultimately hinge upon contextual adaptability, ethical vigilance, and sustained interdisciplinary collaboration. Furthermore, training modules should incorporate role‑play scenarios that simulate spiritual distress, thereby enhancing caregiver competence. Additionally, policy makers ought to recognize spiritual care as a reimbursable service, which could incentivize its systematic adoption. The evolving landscape of digital health also offers opportunities for virtual chaplaincy, a modality that warrants rigorous evaluation. Ultimately, the success of any spiritual intervention rests upon the authenticity of the encounter, a subtle yet decisive factor that no checklist can fully capture.
The checklist is overly simplistic-yes, it lists tasks, but it fails to address the nuanced training needed for staff to deliver genuine spiritual support. Moreover, the lack of measurable outcomes beyond mood ratings makes it difficult to justify resource allocation. In short, without a sturdy evidence base, this looks more like a feel‑good add‑on than a rigorous care component.
Honestly, I think pushing spiritual activities on every dementia patient is a bit much-what if they have no belief system to begin with? It's like forcing a one‑size‑fits‑all solution, and that can be disrespectful. The guide should at least mention the option of secular mindfulness, because not everyone connects with religion. Definately, families need clear guidance on how to respect the individual's wishes.
I really appreciate how the article balances evidence with practical steps; it makes the concept of spiritual care feel accessible. The checklist format is handy for busy caregivers who need a quick reference. I also like the suggestion to use music from the person's youth-it taps into long‑term memory pathways that often stay intact. The emphasis on documenting outcomes is crucial for continuous improvement. Overall, this piece offers a compassionate roadmap without being overly prescriptive.
Oh, sure, because ignoring someone's spiritual needs is never a problem, right? Let's just pretend that all residents are fine with a silent room and call it “personal choice.” Spoiler: many will feel isolated, and that's a real issue you can't sweep under the rug.
Looks like another checklist to add to the pile.
While I understand the concern about simplicity, the checklist is intended as a starter framework rather than an exhaustive protocol. Caregivers can expand each item with tailored activities that respect cultural and individual preferences. Moreover, incorporating measurable mood scales can address the evidence gap you mentioned. It's a flexible tool that invites continual refinement.
Great resource! I especially liked the tip about keeping sessions short-my grandma gets restless after ten minutes. Trying out some gentle hymns this week.
While the optimism is nice, we should remember that not every family has the time or energy to implement all ten items. Prioritizing the most impactful practices, like music therapy, might be more realistic for many households.
Isn't it fascinating how we can turn something as personal as spirituality into a checklist? Yet, I wonder if reducing profound experiences to tick‑boxes does them any justice. Perhaps a hybrid approach, mixing structure with open‑ended reflection, would work better. Anyway, kudos for trying to bring this into mainstream care. Let's see how it plays out in real settings.
Totally agree, ken. The checklist can be a good guide, but flexibility is key. Families should feel free to skip items that don't resonate.
Can't imagine this being adopted in a busy facility-too much paperwork.
The proposal to embed spiritual assessments within the standard intake process is methodologically sound, as it ensures early identification of patient preferences. Empirical studies have demonstrated that early spiritual engagement correlates with reduced neuropsychiatric symptoms, particularly agitation and anxiety. Additionally, the systematic inclusion of chaplaincy referrals can bridge gaps where staff lack theological expertise. From an operational standpoint, integrating a digital checklist into electronic health records minimizes duplication and facilitates longitudinal tracking. It is also prudent to consider the legal implications of documenting spiritual preferences, ensuring compliance with privacy regulations such as HIPAA. Training modules should encompass cultural competency, emphasizing the distinction between religion and broader spirituality. Moreover, the recommendation to employ sensory tools aligns with multisensory integration theories, which posit that concurrent stimulation can reinforce memory pathways. Finally, periodic review cycles, as suggested, enable iterative refinement based on outcome metrics, fostering a culture of continuous improvement.
While the argument for early assessment is compelling, it is essential to recognize the variability in cognitive trajectories among dementia patients. Not all individuals will retain the capacity to articulate spiritual preferences at the point of intake, necessitating adaptive approaches such as proxy reporting by family members. The inclusion of chaplaincy services, albeit beneficial, may encounter logistical constraints, especially in under‑resourced facilities where staffing ratios are already stretched thin. From an informatics perspective, embedding the checklist within existing electronic health record modules requires careful mapping to avoid redundancy and ensure interoperability across platforms. Furthermore, the legal considerations you mention extend beyond mere privacy; they encompass informed consent procedures, particularly when spiritual interventions intersect with medical decision‑making. Training curricula must therefore balance theoretical constructs of cultural competence with pragmatic skill‑building exercises, such as role‑play scenarios that simulate real‑world dilemmas. The use of sensory tools, while grounded in neuroscientific theory, should be individualized to prevent overstimulation, which can paradoxically exacerbate agitation. Finally, the recommendation for periodic reviews aligns with quality improvement frameworks, yet the frequency and metrics for such reviews warrant further specification to avoid audit fatigue.
I think this guide strikes a good balance between being thorough and practical. Care teams can adopt the checklist without feeling overwhelmed.
Agreed, but let's not forget that implementation requires strong leadership and accountability. Without clear directives, even the best checklist can become a wall of paper. I recommend designating a spiritual care champion on each shift to monitor adherence and provide real‑time feedback.
Thanks for the insights! Looking forward to trying some of these ideas.