Ever wondered why the same hydrocortisone cream sometimes seems to work wonders and other times does nothing? The trick isn’t the product itself-it’s how you use it. Below is a no‑fluff guide that walks you through everything you need to know to get the most out of this common topical steroid.
Quick Takeaways
- Use a thin layer; more isn’t better.
- Apply to clean, dry skin and let it absorb before covering.
- Match the cream’s strength to the condition (1% for mild, 2.5% for moderate).
- Pair with a gentle moisturizer to lock in moisture.
- Avoid using on broken skin or for longer than recommended.
What Is Hydrocortisone Cream?
Hydrocortisone Cream is a low‑potency topical steroid that reduces inflammation, itching, and redness on the skin. It works by mimicking the body’s natural cortisol, dampening the immune response that fuels rash and flare‑ups.
Conditions That Benefit From Hydrocortisone
While the cream is sold over the counter in many places, it’s still powerful enough to calm a range of irritations. Typical cases include:
- Eczema - chronic, itchy patches that flare with dryness.
- Psoriasis - thick, scaly plaques that can become red and sore.
- Contact Dermatitis - reactions to allergens or irritants.
- Insect bites, minor burns, and allergic rashes.
For severe or widespread cases, a doctor might prescribe a stronger steroid, but for most everyday flare‑ups, the over‑the‑counter versions do the job.

Choosing the Right Strength
Hydrocortisone comes in several potencies. Picking the correct one avoids under‑treating or over‑exposing your skin.
| Strength | Typical Use | Maximum Daily Duration |
|---|---|---|
| 0.5% | Very mild itch, diaper rash | 7 days |
| 1% | Common eczema, mild psoriasis | 14 days |
| 2.5% | Moderate dermatitis, larger flare‑ups | 7 days (under doctor’s guidance) |
If you’re unsure, start with the lowest effective strength. You can always upgrade if the rash doesn’t improve within a few days.
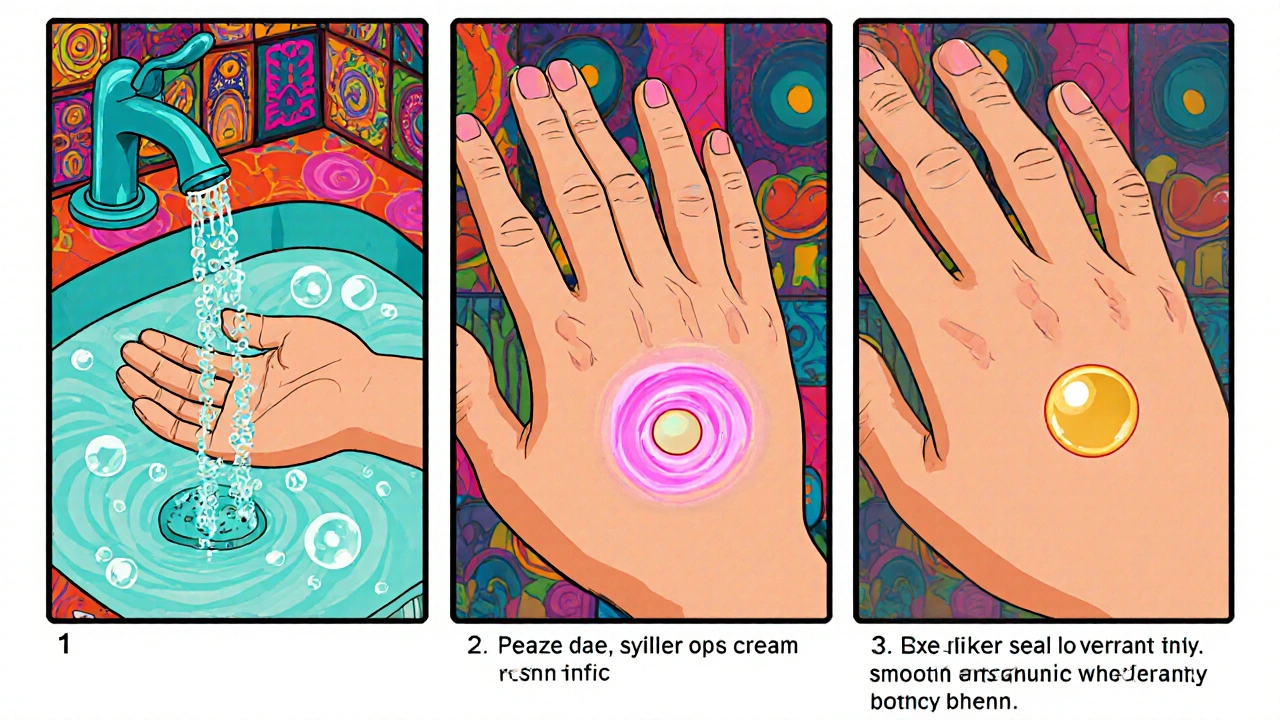
Step‑by‑Step Application Guide
- Wash your hands with mild soap and lukewarm water.
- Gently clean the affected area. Pat dry-don’t rub.
- Apply a pea‑size amount for a small patch or a thin film for larger areas. Less is more.
- Massage lightly for 10-15 seconds until the cream disappears into the skin.
- If you need to bandage, wait 5-10 minutes so the medication can settle.
- Re‑apply only as directed-usually 1-2 times daily.
- Wash hands after each application unless you’re treating your own hands.
Consistency matters more than occasional over‑use. Stick to the schedule and you’ll notice the itch cooling down in a day or two.
Tips to Maximize Results
- Moisturizer after the cream: Once the steroid has been absorbed (about 20 minutes), seal the area with a fragrance‑free moisturizer. This prevents the skin from drying out again.
- Avoid tight clothing that traps heat; cooler skin reduces inflammation.
- Identify triggers-like certain soaps or fabrics-and eliminate them to reduce future flare‑ups.
- For areas prone to rash (e.g., behind knees), apply a thin layer at night to let the skin rest.
- If you’re outdoors, use Sunscreen with at least SPF 30 on top of the moisturizer, because steroids can make skin more sun‑sensitive.
Common Mistakes to Avoid
Even the best product can backfire if you misuse it. Watch out for these pitfalls:
- Using a thick layer-this blocks absorption and can cause a greasy feeling.
- Applying on open wounds or cracked skin; the steroid can be absorbed too quickly.
- Continuing use past the recommended period, which can thin the skin.
- Mixing with other strong topical meds without a doctor’s OK.
- Skipping the moisturizer; dry skin can become itchy again, leading to a cycle of re‑application.
Frequently Asked Questions
Can I use hydrocortisone cream on my face?
Yes, but choose the lowest strength (0.5% or 1%). Apply a tiny amount, avoid the eye area, and limit use to 7‑10 days unless a dermatologist says otherwise.
Is it safe to use hydrocortisone while pregnant?
Low‑potency versions are generally considered safe for short‑term use, but always check with your OB‑GYN before starting any medication.
What should I do if the rash worsens after applying?
Stop using the cream immediately and contact a healthcare professional. Worsening could signal an infection or an allergic reaction to the cream itself.
Can I apply hydrocortisone before bedtime?
Bedtime is a good window because the skin can absorb the medication uninterrupted. Just be sure the area is clean and dry first.
How long does it take to see improvement?
Most people notice itching and redness easing within 24-48 hours. Full clearing of the rash may take 5-7 days, depending on severity.
By following these steps and keeping an eye on the little details, you’ll turn a stubborn rash into a quickly resolved irritation. Remember, the cream does the heavy lifting-but you guide it to where it’s needed.


While the guide provides a solid overview, it neglects several pharmacokinetic subtleties that merit attention. Firstly, the stratum corneum’s lipid composition dictates the percutaneous absorption rate, meaning that occlusive dressings can inadvertently increase systemic exposure. Secondly, the vehicle of the cream-whether anhydrous or water‑based-modulates drug diffusion, a factor often omitted from lay explanations. Moreover, the guideline’s recommendation to apply a "thin layer" lacks quantification; in practice, a pea‑sized amount equates to approximately 0.5 mg cm⁻², a dosage that aligns with FDA‑approved parameters. It is also crucial to emphasize that hydrocortisone’s glucocorticoid receptor affinity, though modest, can still elicit hypothalamic‑pituitary‑adrenal axis suppression if used beyond the stipulated duration. Patients should be counseled to discontinue use promptly if signs of adrenal insufficiency emerge, such as unexplained fatigue or hypotension. Additionally, the interplay between moisturizers and steroid absorption is bidirectional: certain emollients containing petrolatum may prolong drug residence time, whereas aqueous gels could dilute concentration. The article’s omission of contraindications-like fungal infections-poses a risk, as steroids can exacerbate opportunistic pathogens. Lastly, the mention of sunscreen application should be qualified; broad‑spectrum agents with zinc oxide are preferable to avoid phototoxic reactions. In sum, a nuanced approach that integrates these pharmacodynamic and pharmacokinetic considerations will optimize therapeutic outcomes while minimizing adverse effects.
The post does a decent job of covering the basics, but let's be real: most people just slap on a thick blob and call it a day. That "thin layer" advice? It's sound in theory, yet the average user interprets it as "just a dab" and ends up with a greasy mess that barely penetrates. Also, the recommendation to wait 5‑10 minutes before bandaging is optimistic; the skin needs longer to fully absorb the steroid, especially on thicker areas like elbows. Ignoring the potential for steroid‑induced skin atrophy when people over‑apply is a glaring oversight. Bottom line, stick to the schedule and avoid the temptation to double‑dose for faster relief – it rarely works and can backfire.
Great rundown! I love how it stresses moisturizing after the cream – that’s a game‑changer for keeping the skin barrier happy. If you’re dealing with a stubborn eczema flare, try applying a pea‑size amount at night and then a fragrance‑free lotion in the morning. It really helps lock in the medication and reduces the itch cycle. Keep it up!
Honestly the whole "thin layer" thing sounds like an over‑engineered meme the pharma world fed us. Who cares about "pea sized" if the skin is already crying out for relief? The guide pretends to be this holy bible but forgets that real life is messy and you sometimes need a little extra to quiet the fire. Also, the whole moisturizer after‑cream dance is just a marketers’ ploy to sell more lotions. The skin will absorb whatever you put on it, period.
From a pharmacovigilance perspective, the article omits critical risk mitigation strategies, such as monitoring for tachyphylaxis and employing intermittent therapy cycles to preserve epidermal integrity. Additionally, the recommendation to pair hydrocortisone with fragrance‑free moisturizers should be qualified with a discussion of occlusive versus non‑occlusive emollients, as the former can potentiate percutaneous absorption and inadvertently increase systemic exposure. Practitioners must also consider patient‑specific variables, including comorbidities like diabetes mellitus, which may exacerbate steroid‑induced hyperglycemia. The failure to address these nuances undermines the guide's utility for informed clinical decision‑making.
Good points. Make sure hands are clean before applying. Also, limit usage to the recommended days to avoid skin thinning.
There's a philosophical angle here: the cream is merely a tool, the real power lies in the discipline of consistent application. If we treat the regimen as a ritual rather than a quick fix, the mind‑body connection reinforces healing. Over‑reliance on pharmacology without the accompanying behavioral change often leads to relapse. In short, combine the cream with mindful skin care habits and you'll see lasting benefit.
Folks need to wake up to the fact that the mainstream health narrative is pushing these over‑the‑counter steroids to keep us dependent on the pharma pipeline. You think they're just a harmless anti‑itch? No they’re a gateway to systemic cortisol disruption and they’re deliberately downplayed. The guide pretends to be neutral but it's basically a PR piece, glossing over the long term endocrine consequences. Remember the 1990s studies linking topical steroids with subtle adrenal suppression-those aren't mentioned. Stay vigilant, question the dosage recommendations, and consider natural alternatives before buying into the chemical quick‑fix.
i think u r overthinking it theres no big conjur gconspiracy behind a simple cream its just a med and u can use it safe as long as u follow the label
Wow, what a drama about a cream.
Nice guide! I’ve been using the 1% for my kid’s eczema and adding a light moisturizer right after really helped keep the itch down.
Happy to see a straightforward explanation. For anyone new, remember to test a small patch first to ensure no allergic reaction before full application.
OMG, thank you!! 🎉 I was so scared to try a steroid on my face, but your tip about low‑strength (0.5% max) and a tiny dab made me feel sooo much better. I literally saw the redness fade in two days. Also, the suggestion to pair it with a fragrance‑free moisturizer? Genius! I’m definitely keeping this routine forever now.
Hey all, just wanted to add that if you’re dealing with a rash near a joint, a gentle squeeze of the cream into the crease and then a short 5‑minute wait before dressing can prevent that sticky feeling. Also, don’t forget to reapply after a shower – the water can rinse off some of the product.