When you or someone you love is dealing with inflammatory bowel disease (IBD), the medication choice can feel like a maze. Entocort (budesonide) often shows up as a go‑to option, but there are several other drugs that promise similar relief. This guide breaks down how Entocort stacks up against the most common alternatives, so you can decide which pill, capsule, or injection fits your health goals and lifestyle.
What is Entocort (Budesonide)?
Entocort is a controlled‑release oral capsule that contains budesonide, a locally acting glucocorticoid. It was approved by the FDA in 2002 for the treatment of mild to moderate Crohn’s disease affecting the ileum and right colon. By releasing the steroid directly in the gut, Entocort minimizes systemic absorption, which translates into fewer classic steroid side effects like weight gain or bone loss.
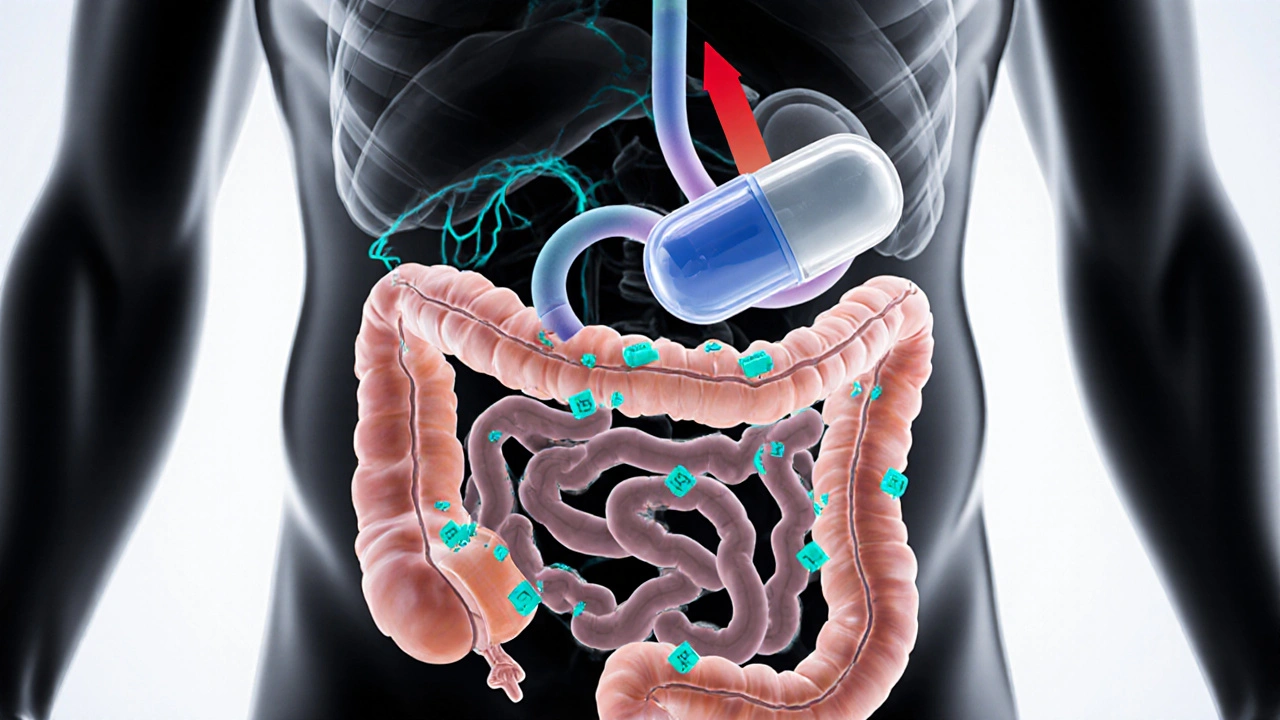
How Entocort Works Inside the Body
Budesonide binds to glucocorticoid receptors in the intestinal lining, dampening the inflammatory cascade that damages the mucosa. Because the drug is formulated to dissolve in the distal small intestine, it concentrates where Crohn’s lesions often appear. The result is a rapid reduction in abdominal pain, diarrhea, and fatigue, typically within 2‑4 weeks of starting therapy.
Key Alternatives to Entocort
Below are the most frequently prescribed IBD medications that patients consider instead of Entocort. Each has a distinct mechanism, delivery method, and safety profile.
- Prednisone - a systemic oral corticosteroid that suppresses inflammation throughout the body.
- Mesalamine (also known as 5‑ASA) - an anti‑inflammatory agent delivered via tablets, suppositories, or enemas.
- Adalimumab - a biologic monoclonal antibody that blocks tumor necrosis factor‑α (TNF‑α).
- Uceris - a brand of budesonide formulated as a rectal foam for ulcerative colitis.
Side‑by‑Side Comparison Table
| Drug | Class | Delivery | Typical Dose | Onset of Relief | Common Side Effects | Average Annual US Cost |
|---|---|---|---|---|---|---|
| Entocort (budesonide) | Topical glucocorticoid | Oral capsule | 9mg daily (divided) | 2‑4 weeks | Mild thrush, headache | $2,800 |
| Prednisone | Systemic glucocorticoid | Oral tablet | 20‑40mg daily (taper) | 1‑2 weeks | Weight gain, insomnia, hypertension | $150 |
| Mesalamine | 5‑ASA anti‑inflammatory | Tablet / suppository / enema | 2‑4g/day | 4‑6 weeks | Nausea, headache, rash | $1,200 |
| Adalimumab | TNF‑α inhibitor (biologic) | Subcutaneous injection | 40mg every 2 weeks | 6‑8 weeks | Injection site reaction, infection risk | $45,000 |
| Uceris (budesonide foam) | Topical glucocorticoid | Rectal foam | 2mg once daily | 2‑3 weeks | Rectal irritation, mild systemic effects | $3,400 |
When Entocort Is the Right Choice
If your diagnosis is Crohn’s disease limited to the ileum or right colon, Entocort’s targeted release gives you high local potency with low systemic risk. It’s especially appealing for patients who have already tried mesalamine without success but want to avoid the heavy‑handedness of prednisone.
When to Consider an Alternative
- Extensive disease - If inflammation spreads beyond the distal small intestine, a systemic steroid like prednisone may reach affected areas faster.
- Severe flares - Biologics such as adalimumab are often reserved for patients with refractory disease or frequent hospitalizations.
- Ulcerative colitis - For colonic disease, rectal formulations (Uceris) or oral mesalamine tend to work better than an ileal‑focused budesonide capsule.
- Cost constraints - Generic prednisone and mesalamine are far cheaper than branded budesonide or biologics, which matters for long‑term therapy.
Safety Profile: What to Watch For
Even though budesonide is “locally acting,” long‑term use can still lead to adrenal suppression, especially at higher doses (>12mg/day). Periodic morning cortisol testing is advised for patients on continuous therapy beyond 3 months.
Prednisone carries a well‑known list of systemic effects: osteoporosis, glucose intolerance, cataracts, and mood swings. If you need a short burst (<2 weeks), the benefits often outweigh the risks, but a taper plan is essential to avoid rebound inflammation.
Biologics such as adalimumab demand vigilant infection screening. Patients must be tested for latent TB and hepatitis B before the first injection, and regular skin checks are recommended because of the rare risk of lymphoma.
Cost Considerations and Insurance Navigation
Insurance formularies vary widely. Many plans place Entocort on a higher tier than generic prednisone, meaning higher co‑pays. However, some pharmacy benefit managers offer patient assistance programs that can reduce the out‑of‑pocket cost to under $50 per month.
Biologics are usually covered under specialty pharmacy benefits, which can involve prior authorization and a $5,000‑plus annual deductible. If cost is a major barrier, ask your gastroenterologist about step‑up therapy: start with mesalamine, add budesonide if needed, and reserve biologics for flare‑unresponsive cases.
Decision Checklist - Pick the Best Option for You
- Identify disease location: ileum/right colon vs. extensive colon.
- Assess severity: mild‑moderate vs. severe/refractory.
- Consider timeframe: need rapid relief or can wait 4‑6 weeks?
- Review side‑effect tolerance: systemic steroid side effects vs. biologic infection risk.
- Check insurance coverage and patient assistance options.
- Discuss with your gastroenterologist about a taper plan if you start a steroid.
- Schedule regular monitoring (cortisol levels, bone density, infection labs).
Practical Tips for Getting the Most Out of Your Medication
- Take Entocort capsules with a full glass of water, preferably at the same time each day to maintain steady gut exposure.
- If you miss a dose, take it as soon as you remember unless it’s within 12hours of the next scheduled dose - then skip and resume the regular schedule.
- Combine budesonide with a probiotic (e.g.,Lactobacillusreuteri) to support gut flora and potentially reduce diarrhea.
- Track symptoms in a diary: stool frequency, abdominal pain score, and energy level. This data helps your doctor decide when to step down or up therapy.
- For biologic injections, rotate injection sites (abdomen, thigh, upper arm) to minimize skin irritation.
Frequently Asked Questions
Can I use Entocort for ulcerative colitis?
Entocort is formulated to release budesonide in the terminal ileum and right colon, so it’s not the first‑line choice for extensive ulcerative colitis. For colonic disease, rectal budesonide (Uceris) or oral 5‑ASA agents work better.
How long can I stay on Entocort?
Most guidelines recommend using Entocort for up to 12 weeks as induction therapy. If symptoms stay controlled, a physician may prescribe a maintenance dose (usually 3mg daily) for longer periods, but periodic cortisol testing is advisable.
Is budesonide safer than prednisone?
Because budesonide undergoes extensive first‑pass metabolism, systemic exposure is roughly 10‑20% of that from prednisone at equivalent anti‑inflammatory doses. This translates to fewer classic steroid side effects, though adrenal suppression can still occur at high or prolonged dosing.
What should I do if I experience a flare while on Entocort?
Contact your gastroenterology team right away. They may add a short course of prednisone, increase the budesonide dose temporarily, or consider stepping up to a biologic if flares become frequent.
Can I take probiotics together with Entocort?
Yes, probiotics are generally safe and may help rebalance gut flora after steroid therapy. Choose a strain‑specific product with clinical data for IBD, such asLactobacillusreuteri DSM 17938.

In the grand theater of IBD treatment, Entocort strides onto the stage like a brooding protagonist, cloaked in the subtlety of localized steroids. Its release mechanism whispers promises of relief while the rest of the body watches, untouched by the usual steroidic chaos. Yet, every hero bears a shadow, and the occasional thrush or headache is the echo of that silent battle. The choice, dear reader, is a plot twist waiting to be written.
This whole thing is just a corporate cash grab.
When you examine the landscape of inflammatory bowel disease therapeutics you quickly realize that the United States has long been a crucible for pharmaceutical innovation and that Entocort represents one of those homegrown attempts to balance efficacy with safety in a market saturated with both generic and brand‑name competitors the drug’s targeted release mechanism is designed to deposit budesonide directly into the distal ileum thereby reducing systemic exposure and that feature alone distinguishes it from the blunt force of systemic prednisone however the reality remains that no oral formulation can completely escape the body’s absorptive pathways and long‑term users must remain vigilant for signs of adrenal suppression and that vigilance is a responsibility that falls squarely on the patient and their clinician alike the cost profile of Entocort, while modest compared to biologics, still exceeds that of generic prednisone by a wide margin and that price gap can be a decisive factor for many American families especially those without comprehensive insurance coverage the comparative data suggests that mesalamine, despite its slower onset, offers a favorable safety record with fewer endocrine disturbances yet its efficacy is limited to certain disease locations which means that it cannot universally replace a targeted steroid in Crohn’s disease limited to the ileum the decision matrix thus becomes a complex interplay of disease extent, patient preference, comorbidities, and financial considerations and in this intricate calculus the physician’s role is not merely to prescribe but to educate and to tailor therapy to the individual while also navigating the regulatory environment that governs drug approvals and insurance formularies the American healthcare system, with all its flaws, still manages to provide access to these therapies for a majority of patients but the out‑of‑pocket burden can be crippling for the underinsured individuals the emerging biosimilar market may eventually bring down the cost of biologics but until that shift occurs Entocort remains a viable middle ground for certain Crohn’s presentations the takeaway, if you will, is that there is no universal answer and that each therapeutic choice carries its own constellation of benefits and drawbacks you must weigh them carefully
From a philosophical standpoint the selection of an IBD agent is a manifestation of the broader American pursuit of individualized liberty within the constraints of medical science. Entocort embodies a compromise, delivering potent local immunosuppression whilst preserving systemic integrity-a balance that resonates with our national ethos of efficiency and restraint. Nevertheless, the specter of cost looms, reminding us that fiscal responsibility remains a cornerstone of our collective health policy. In comparing alternatives, one must consider not merely pharmacology but also the societal impact of widespread drug expenditures. Ultimately, the prudent clinician will weigh these dimensions with a precision befitting the American tradition of rigorous analysis.
Entocort arrives like a dramatic hero on the stage of treatment but the cost drama follows close behind this drug promises local relief yet the numbers whisper caution many patients feel the sting of price without the safety of a simple pill
Hey folks, I get that sifting through all these meds can feel like wading through a swamp-so here’s a little lighthouse: if your Crohn’s is stuck in the ileum, give Entocort a solid try, it usually gives relief without the whole-body steroid side effects. Keep an eye on any odd thursh or headaches, and don’t forget to get your cortisol checked after a few months. And remember, the cheapest option isn’t always the best if it leaves you feeling worse-talk to your doc, share your concerns, and together you’ll find a plan that works for you.
I have to say that the whole conversation around Entocort versus other IBD drugs often gets blown out of proportion and people forget the basic facts that matter most to us. First of all, the drug is designed to work where the disease is most active and that is a real advantage over something like prednisone that just floods the whole body. Second, the side‑effects are generally milder which means patients can stay on it longer without the scary bone loss or weight gain. Third, the price is still high but when you compare it to biologics you are actually saving a lot of money. Fourth, the administration is simple-you just swallow a capsule instead of dealing with injections. Fifth, if you have disease limited to the ileum you should absolutely consider Entocort before jumping straight to the more aggressive therapies.
Let's cut the fluff: Entocort is a gimmick wrapped in a fancy capsule, a half‑hearted attempt to mask the fact that it still delivers steroids to your gut. The real winners are the cheap steroids and the mighty biologics that actually change the disease course-anyone who thinks this mild budesonide can replace them is living in denial. And don't get me started on the price tag, it's a robbery disguised as innovation. Bottom line: if you want real control, you either go full‑blast prednisone or jump straight to anti‑TNF agents.
Well, actually the studies do show that budesonide has a statistically significant benefit in ileal Crohn’s, so dismissing it outright ignores the data. Maybe you should read the latest guidelines before throwing shade.
Just to add, the bioavailability of budesonide is about 10‑15% because of the first‑pass effect, which is why systemic side effects are lower. Also, the dosing schedule can be flexible-you can split the 9 mg into 3 mg three times a day if that helps adherence. Keep in mind drug interactions, especially with CYP3A4 inhibitors.
Your encouragement is appreciated but patients should be warned that even mild steroids can suppress the hypothalamic‑pituitary‑adrenal axis if used long‑term. It’s crucial to schedule periodic cortisol assessments.
Remember, you’re not alone in navigating these options-talk to a gastroenterology specialist, join a patient support group, and keep a symptom diary to track how each medication affects you. Consistency and open communication are key to finding the right balance.
Upon rigorous examination of the pharmacoeconomic data, it becomes evident that Entocort's cost‑effectiveness ratio is inferior to that of generic prednisone when evaluated through the lens of quality‑adjusted life years. Consequently, prescribing practices should prioritize agents with demonstrable economic and clinical superiority.
I hear how overwhelming all these choices can feel, and it’s okay to take your time researching each option. Sharing your concerns with your healthcare team can lead to a tailored plan that respects both your health goals and your budget.
Ah, the dazzling tableau of IBD therapeutics! One glimpses Entocort as the modest artisan amidst the gilded biopharma colossi, a subtle brushstroke upon the canvas of mucosal inflammation.
I’m all for being assertive with your doctor-ask about budesonide’s adrenal suppression risk and demand a clear tapering plan if you’re on it long term. Also, push for insurance coverage options before you sign up for a pricey biologic. Your health decisions deserve that level of advocacy.