Hypertension Medication Decision Aid
Select Your Health Factors
Answer these questions to get personalized recommendations for hypertension medications
Key Takeaways
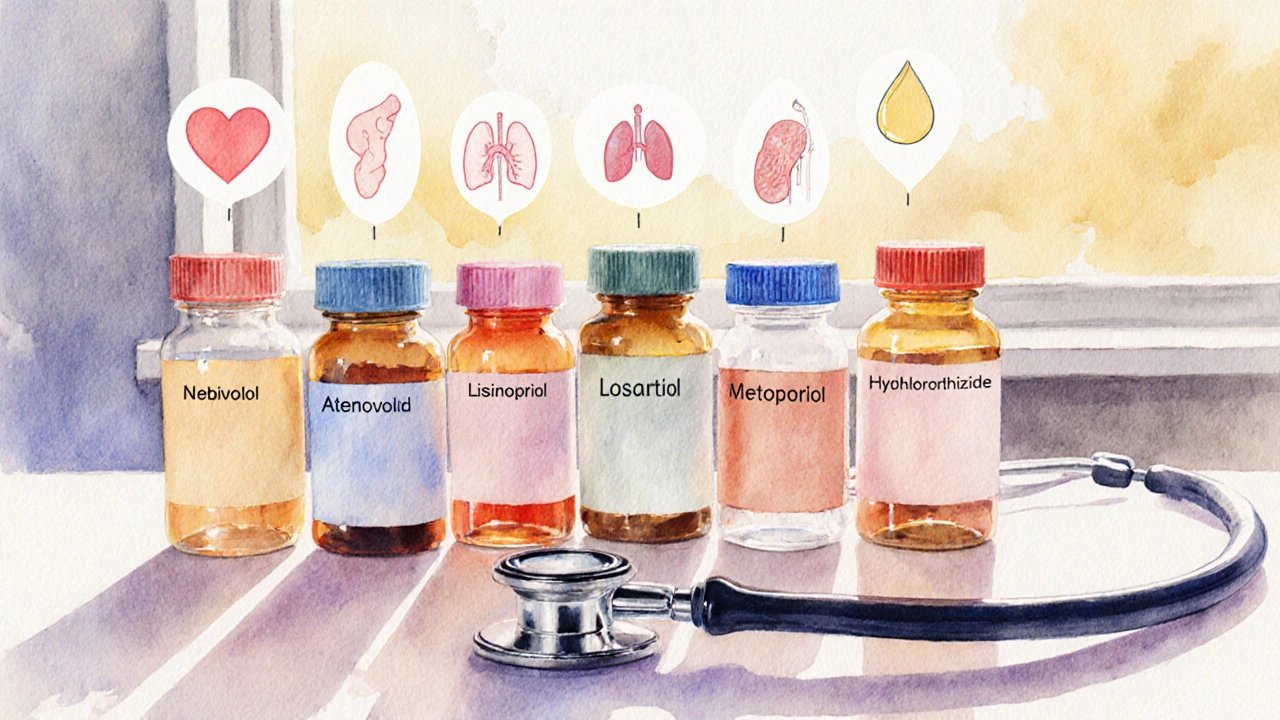
- Nebivolol (Bystolic) is a beta‑blocker that also boosts nitric oxide, helping lower blood pressure with fewer typical beta‑blocker side effects.
- Common alternatives include atenolol, lisinopril, losartan, carvedilol and metoprolol, each with distinct mechanisms and dosing nuances.
- When choosing, consider factors like heart rate impact, metabolic effects, cost, and how the drug fits with existing conditions.
- Side‑effect profiles differ: Bystolic often causes less fatigue than older beta‑blockers, while ACE inhibitors may trigger cough.
- Always discuss with a healthcare provider before switching; a gradual taper may be needed for beta‑blockers.
When it comes to controlling hypertension, Bystolic is frequently mentioned, but many patients wonder how it stacks up against other options. This guide walks you through the science behind nebivolol, compares it side‑by‑side with the most common alternatives, and gives you clear criteria to decide which drug might fit your lifestyle and health profile.
Bystolic is the brand name for nebivolol, a third‑generation beta‑blocker that uniquely stimulates nitric oxide release while blocking beta‑1 receptors. Approved by the FDA in 2007, it’s prescribed for adults with primary hypertension and can be part of a broader cardiovascular regimen.
How Nebivolol (Bystolic) Lowers Blood Pressure
Traditional beta‑blockers, like atenolol or metoprolol, primarily slow the heart rate and reduce cardiac output. Nebivolol adds a second mechanism: it activates endothelial nitric oxide synthase, which relaxes blood vessels and improves arterial compliance. The dual action often translates to a modest reduction in heart rate without the pronounced fatigue seen in older beta‑blockers.
Typical dosing starts at 5mg once daily, with a maximum of 40mg for resistant cases. The drug is metabolized mainly by CYP2D6; poor metabolizers may need a lower dose to avoid excessive plasma levels. Because nebivolol is highly selective for beta‑1 receptors, it spares beta‑2 receptors in the lungs, making it a safer choice for patients with mild asthma.
Common Alternatives to Bystolic
Below are the most prescribed hypertension drugs that patients often compare to nebivolol. Each brief description includes the drug class, typical dose range, and one key attribute that distinguishes it.
Atenolol is a first‑generation beta‑blocker that blocks beta‑1 receptors without nitric oxide activity. It’s inexpensive and widely used, but can cause noticeable fatigue and cold extremities.
Lisinopril belongs to the ACE‑inhibitor class, preventing angiotensin‑II formation. It lowers blood pressure by dilating arteries and is especially helpful for patients with diabetic kidney disease. A common side effect is a dry cough.
Losartan is an angiotensinII receptor blocker (ARB). It offers similar benefits to ACE inhibitors but with a lower incidence of cough, making it a go‑to for patients who can’t tolerate lisinopril.
Carvedilol combines non‑selective beta‑blockade with alpha‑1 blocking activity, providing vasodilation alongside heart‑rate reduction. It is often chosen for patients with both hypertension and heart failure.
Metoprolol is a cardioselective beta‑blocker that is available in immediate‑release and extended‑release forms. It’s a solid middle‑ground option but does not have nebivolol’s nitric‑oxide benefit.
Hydrochlorothiazide is a thiazide diuretic that reduces blood volume by increasing urinary sodium and water excretion. Often paired with a beta‑blocker, it helps achieve target pressures in resistant cases.
Side‑Effect Profile at a Glance
| Drug | Common Side Effects | Serious Risks | Typical Cost (US, 30‑day supply) |
|---|---|---|---|
| Bystolic (Nebivolol) | Headache, mild fatigue, dizziness | Bradycardia, bronchospasm in severe asthma | $30‑$45 (generic) |
| Atenolol | Fatigue, cold hands/feet, depression | Severe bradycardia, heart block | $10‑$20 |
| Lisinopril | Cough, elevated potassium, dizziness | Angio‑edema, renal impairment | $15‑$25 |
| Losartan | Dizziness, nasal congestion | Kidney injury, hyperkalemia | $20‑$35 |
| Carvedilol | Fatigue, weight gain, dizziness | Worsening heart failure if started too high | $25‑$40 |
| Metoprolol | Fatigue, insomnia, respiratory issues | Severe bradycardia, bronchospasm | $15‑$30 |
| Hydrochlorothiazide | Increased urination, electrolyte loss | Severe hyponatremia, gout flare | $5‑$15 |
Decision Criteria: Which Drug Fits Your Situation?
Choosing a hypertension med isn’t a one‑size‑fits‑all exercise. Below are the main factors you should weigh, illustrated with how nebivolol and its peers line up.
- Heart‑Rate Control: If you need a low resting heart rate, beta‑blockers (nebivolol, atenolol, metoprolol, carvedilol) excel. Nebivolol’s nitric‑oxide boost means you can achieve target pressure without overly suppressing heart rate.
- Metabolic Impact: Some beta‑blockers worsen lipid profiles or glucose tolerance. Nebivolol has a neutral or slightly positive effect on metabolism, making it a better choice for patients with metabolic syndrome.
- Respiratory Concerns: For mild asthma, a cardioselective agent like nebivolol or metoprolol is safer than non‑selective carvedilol.
- Kidney Health: ACE inhibitors (lisinopril) and ARBs (losartan) protect kidney function in diabetics. If you have diabetic nephropathy, these may be preferred over beta‑blockers.
- Side‑Effect Tolerance: If a chronic cough is a deal‑breaker, avoid lisinopril and consider losartan or a beta‑blocker.
- Cost & Insurance Coverage: Generic versions of atenolol and hydrochlorothiazide are cheapest; nebivolol’s price has dropped since generic approval, but still sits a bit higher.
Practical Tips for Starting or Switching
- Start Low, Go Slow: Begin nebivolol at 5mg once daily. If blood pressure remains above target after 2‑4 weeks, the dose can be doubled.
- Watch for Interactions: Nebivolol is metabolized by CYP2D6. Drugs that inhibit this enzyme (e.g., fluoxetine, quinidine) may raise nebivolol levels.
- Monitor Heart Rate: Aim for a resting rate of 60‑70bpm. If it drops below 50bpm, inform your doctor-dose adjustment may be needed.
- Tapering Beta‑Blockers: Never stop nebivolol abruptly. Reduce the dose by 25% every week to avoid rebound hypertension.
- Combine Wisely: Pairing nebivolol with a low‑dose thiazide (hydrochlorothiazide) often achieves better control without excessive dosing.
- Pregnancy & Breastfeeding: Data are limited. Generally, ACE inhibitors and ARBs are avoided; beta‑blockers like nebivolol may be used only if benefits outweigh risks.
When Bystolic Might Not Be the Best Choice
Even though nebivolol has a favorable side‑effect profile, there are scenarios where alternatives shine:
- Severe Congestive Heart Failure: Carvedilol’s combined alpha‑ and beta‑blockade provides extra afterload reduction.
- Diabetic Kidney Disease: ACE inhibitors or ARBs slow microalbuminuria progression better than beta‑blockers alone.
- Cost‑Sensitive Patients: Atenolol and hydrochlorothiazide are substantially cheaper and widely covered.
- Patients with Bradycardia at Baseline: Starting a beta‑blocker could push the heart rate too low; an ARB or diuretic might be safer.
Bottom Line
Nebivolol (Bystolic) offers a modern twist on beta‑blockade by adding nitric‑oxide‑mediated vasodilation. This means effective blood‑pressure control with a gentler side‑effect slate for many patients. However, the “best” drug still depends on the individual’s other health conditions, tolerance for side effects, and financial situation. Use the comparison table and decision criteria above to have an informed conversation with your clinician.
Frequently Asked Questions
Can I take Bystolic with a diuretic?
Yes. Combining nebivolol with a thiazide diuretic (like hydrochlorothiazide) is a common strategy to hit target blood‑pressure numbers faster, as they work on different pathways.
What makes nebivolol different from atenolol?
Nebivolol is a third‑generation beta‑blocker that also releases nitric oxide, leading to vessel relaxation. Atenolol blocks beta‑1 receptors only and lacks this vasodilatory effect, often resulting in more fatigue.
Is Bystolic safe for people with mild asthma?
Because nebivolol is highly cardio‑selective, it spares beta‑2 receptors in the lungs. Most patients with mild asthma tolerate it well, but severe asthma still warrants caution.
How long does it take to see blood‑pressure improvement?
Patients usually notice a drop within 2‑4 weeks of consistent dosing. Full therapeutic effect may take up to 8 weeks, especially if the dose is being titrated.
Can I switch from lisinopril to Bystolic without a wash‑out period?
A short overlap is often acceptable, but your doctor might stagger the change to monitor blood pressure and kidney function. Never discontinue an ACE inhibitor abruptly without medical guidance.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one-don’t double‑dose.


In the landscape of antihypertensive therapy, nebivolol occupies a nuanced position that merits careful contemplation. Its dual mechanism-beta‑1 blockade coupled with nitric‑oxide mediated vasodilation-offers a subtle advantage over traditional agents. Patients who prioritize cardiovascular protection without pronounced fatigue may find this profile appealing. Nevertheless, the choice must be contextualized within comorbidities such as diabetes or renal impairment. A measured discussion with one’s clinician remains indispensable.
Honestly the article glosses over the harsh reality that nebivolol is just another overpriced brand name drug that many insurers refuse to cover It pretends to be special because it releases nitric oxide but the clinical benefit is marginal The cost alone makes it a poor first‑line choice for most patients especially when generic alternatives exist The supposed “less fatigue” claim is anecdotal at best and ignores the fact that beta‑blockers universally lower heart rate which can be detrimental for active individuals Moreover the safety data in severe asthma is not as robust as the author suggests In short the hype outweighs the modest advantages
The pharmacokinetic profile of nebivolol is characterized by extensive first‑pass metabolism via CYP2D6, yielding a substrate‑dependent variability that necessitates phenotypic stratification in clinical algorithmic decision‑making. Hemodynamically, the agent exerts negative chronotropy while simultaneously augmenting endothelial nitric oxide synthase activity, thereby effecting arterial compliance improvement. This synergistic modality can be particularly advantageous in patients with isolated systolic hypertension where pulse pressure reduction is paramount. However, the drug‑drug interaction matrix, especially with potent CYP2D6 inhibitors, mandates vigilant therapeutic drug monitoring to preempt supratherapeutic plasma concentrations. Consequently, while nebivolol offers a mechanistic edge, its deployment should be predicated on a comprehensive risk‑benefit assessment.
Hey, great points about the metabolism stuff. For most folks just starting on blood pressure meds, nebivolol can feel smoother than the older beta‑blockers. It’s less likely to make you feel wiped out, which is a big win if you’re juggling work and family. Just keep an eye on your heart rate and let your doc adjust the dose if needed. Overall, it’s a solid option for a lot of people.
While everyone raves about “modern” drugs the truth is that the oldest beta‑blockers have stood the test of time and still deliver reliable outcomes The newer agents like nebivolol are marketed hype rather than true innovation The nitric oxide angle sounds fancy but adds little real‑world benefit when you compare mortality data across classes Moreover, the push for newer patents benefits pharma more than patients who could be saved money on tried‑and‑true generics
Thank you for sharing that perspective. It is indeed important to remember that long‑standing medications have a robust evidence base. At the same time, individual patient factors-such as asthma severity or metabolic concerns-may justify exploring newer options like nebivolol. Shared decision‑making with a healthcare professional can help balance these considerations. Your comment highlights the need for a personalized approach.
Did you ever wonder why the pharma giants keep pushing nebivolol as the "miracle" beta‑blocker? It's all part of a larger scheme to keep us dependent on brand‑name drugs that cost more than a simple cheap pill. They hide the fact that most of the benefits are just marketing fluff while the real data is buried deep in pay‑walled journals. Trust the system? Not really. Stay skeptical and question every "new" hype.
Look I get the complxities but the article is just a fluff piece It pretends nebivolol is some superhero but the side effcts are still there Like any beta blocker you can get fatigue and bradycardia If you ignore thos you might end up woth a worse outcome So keep it real and read the fine print.
Wow!!! This guide really blew my mind!!! 😮💨 The comparison tables are so helpful!!! I love how the author took the time to lay out every little side‑effect!!! It’s like a treasure trove of info!!! 🙌
Indeed, the detailed side‑effect matrix is a valuable resource 😊 While the tone remains quite measured, the inclusion of clear tables aids comprehension. Patients can better weigh pros and cons before consulting their physician. 👍
Excellent post! The formatting is clean, and the information is presented logically. I appreciate the consistent use of proper punctuation and spelling throughout. Kudos to the author for maintaining high editorial standards.
Sure, but don't forget that most of these "expert" articles are funded by the same companies that sell the meds :) Keep an eye on hidden agendas! ;)
Reading through this exhaustive comparison felt like embarking on an epic odyssey through the labyrinthine world of hypertension therapeutics, each paragraph unveiling another layer of complexity that could make even a seasoned cardiologist pause for breath. The author daringly juxtaposes nebivolol-a drug that some claim is the silver bullet of blood pressure control-with a cavalcade of older, time‑tested agents, painting a picture that is both awe‑inspiring and, frankly, a tad overwhelming. One cannot help but notice the meticulous attention to detail, from the nuanced discussion of nitric oxide pathways to the painstaking enumeration of side‑effect frequencies, which reads like a saga of pharmacological intrigue. Yet, amid this torrent of data, there is a subtle undercurrent of elitism, as if the mere act of reading the article confers a badge of superior medical literacy. The tables, while impeccably styled, seem to whisper that only the truly diligent will decipher their hidden meanings, leaving the casual reader adrift in a sea of numbers. Moreover, the narrative intermittently drifts into melodramatic flair, describing fatigue as if it were a tragic heroine whose demise could be averted solely by choosing the “right” pill. It is almost as if the writer fears that without this grandiose exposition, the audience might dismiss the importance of nuanced decision‑making. The emphasis on cost, for instance, is presented with such gravitas that one imagines an entire economy hinging on the price of a 30‑day supply. While this dramatization can be engaging, it occasionally borders on hyperbole, especially when the piece declares nebivolol as the “ultimate solution” for patients with mild asthma-an assertion that, in reality, warrants cautious optimism rather than unbridled acclaim. Still, the author’s dedication to covering every conceivable angle-from metabolic effects to patient adherence-cannot be denied, and it does foster a sense of thoroughness that many would envy. The occasional use of bolded subheadings acts as a beacon, guiding the reader through the dense forest of clinical considerations. In the end, despite the occasional theatrical flourish, the article succeeds in delivering a comprehensive snapshot that empowers patients to engage in informed conversations with their providers. One leaves the page feeling both enlightened and slightly exhausted, as though having trekked across a mountainous terrain of pharmacology. Ultimately, the piece stands as a testament to the complexities inherent in modern hypertension management, reminding us that the journey to optimal blood pressure control is rarely a straight line but a winding road filled with twists, turns, and occasional dramatic pauses.
Great summary, Rhonda. Concise overview: nebivolol offers benefits but patient selection is key.
Nice, another drug to pretend we didn't already have enough.
We must remember that prescribing decisions carry ethical weight and should not be driven by marketing hype 😠 Patients deserve transparent information and equitable access to care 🌍