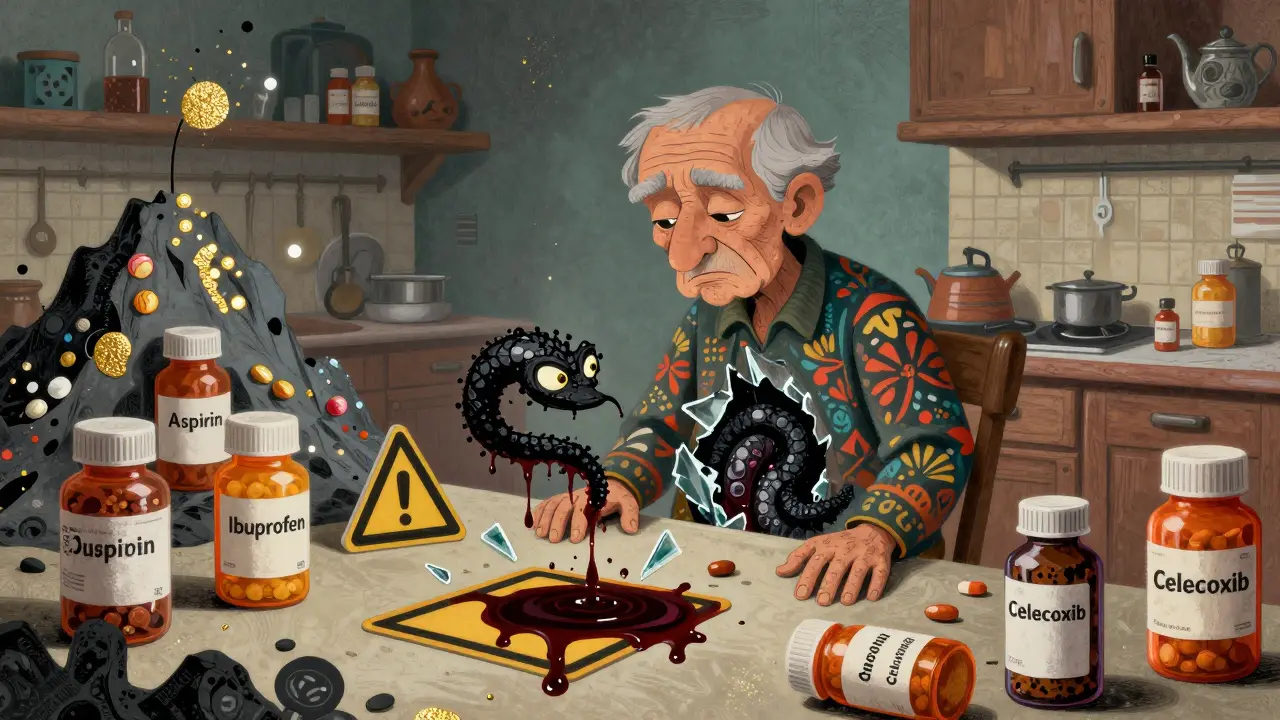
Every year, thousands of people end up in the hospital not from a fall, a car crash, or a bad infection-but from something they took to feel better. NSAID overdose isn’t always about swallowing a whole bottle. Often, it’s just taking too much for too long-daily ibuprofen for back pain, aspirin for heart health, naproxen for arthritis-and not realizing how quietly it’s eating away at your gut.
What Happens When NSAIDs Attack Your Stomach
NSAIDs-like ibuprofen, naproxen, aspirin, and celecoxib-are designed to block pain and inflammation. But they don’t know the difference between the inflammation in your knee and the protective lining in your stomach. When you take them regularly, they strip away the mucus that shields your stomach and intestines from acid. Over time, this leads to tiny tears, then ulcers, then bleeding.You might not feel it at first. In fact, up to 70% of long-term NSAID users show signs of damage on an endoscopy-erosions, ulcers, bleeding-while only 10% report any symptoms like heartburn or stomach pain. That’s the silent danger. By the time you notice black, tarry stools or feel dizzy from blood loss, the damage is already severe.
Studies show NSAID users are four times more likely to have a gastrointestinal bleed than people who don’t take them. And it’s not just prescription pills. Over-the-counter aspirin, often taken daily for heart protection, raises your risk of bleeding by 2 to 4 times. One study found that over one-third of people admitted for GI bleeding were taking low-dose aspirin they bought without a prescription.
Who’s Most at Risk
Not everyone who takes NSAIDs bleeds. But some people are walking into a minefield without knowing it.- People over 65: Your stomach lining thins with age. Even a single daily aspirin can be dangerous.
- Those with a history of ulcers or bleeding: If you’ve had a bleed before, your chance of another one is dramatically higher.
- People on blood thinners or antiplatelets: Taking aspirin plus another blood thinner like clopidogrel? That combination doubles your risk of bleeding.
- Those with H. pylori infection: This common stomach bacteria works with NSAIDs to make ulcers form faster and bleed more easily.
- People taking multiple NSAIDs: Ibuprofen at breakfast, naproxen at night, and aspirin for heart health? That’s a recipe for disaster.
And here’s the kicker: enteric-coated or buffered aspirin doesn’t help. It’s still absorbed in your gut and still damages the lining. Same goes for COX-2 inhibitors like celecoxib-they’re not magic shields. If you’re on low-dose aspirin, adding a COX-2 inhibitor doesn’t reduce your bleeding risk. It just gives you a false sense of safety.
The Hidden Signs You’re Bleeding Inside
Most people think GI bleeding means vomiting blood or passing bright red stool. But that’s the rare kind. The more common-and dangerous-kind is slow, silent bleeding.- Iron deficiency anemia: You feel tired, short of breath, or pale. Your doctor says your hemoglobin is low. They check your diet, your periods, your colon-but never think to ask about your painkillers. In clinical trials, over half of NSAID users became anemic without any visible bleeding.
- Black, sticky stools: That’s melena-digested blood. It smells foul, like tar. Don’t ignore it. It’s not just from eating blueberries.
- Unexplained fatigue or dizziness: If you’re losing blood slowly, your body can’t keep up. You might chalk it up to stress or aging, but it could be your stomach bleeding out.
- Heartburn that won’t go away: Not all reflux is acid. Sometimes it’s a warning sign your stomach lining is breaking down.
Here’s the truth: if you’ve been taking NSAIDs for more than a few weeks and you’re over 50, you should be screened-even if you feel fine. A simple blood test for hemoglobin and iron levels can catch bleeding before it becomes an emergency.
How to Protect Yourself
The good news? This isn’t inevitable. You can take control.- Use the lowest dose for the shortest time: If you’re taking ibuprofen daily for back pain, ask yourself: Do you really need it? Could stretching, heat, or physical therapy help instead?
- Never combine NSAIDs: No ibuprofen with naproxen. No aspirin with Aleve. Even one OTC NSAID plus a prescription NSAID is risky.
- Talk to your doctor before taking aspirin daily: If you’re over 60 and have no history of heart disease, daily aspirin might do more harm than good. The risks of bleeding often outweigh the benefits.
- Ask about PPIs if you must take NSAIDs long-term: Proton pump inhibitors like omeprazole can help protect your stomach-but they don’t fix damage in your small intestine. They’re not a cure-all, but they’re better than nothing for high-risk people.
- Get tested for H. pylori: If you’ve had an ulcer or are on long-term NSAIDs, ask for a breath or stool test. Treating this infection cuts your bleeding risk in half.
- Know your meds: Many heart medications, antidepressants, and steroids also raise bleeding risk. Make sure your doctor knows everything you’re taking.
When to Go to the ER
Don’t wait for symptoms to get worse. If you have any of these, seek help immediately:- Black, tarry, or bloody stools
- Vomiting blood or material that looks like coffee grounds
- Sudden dizziness, fainting, or rapid heartbeat
- Severe abdominal pain with weakness
These aren’t signs to "wait and see." GI bleeding can turn deadly in hours. Emergency treatment includes blood transfusions, endoscopy to find and stop the bleed, and stopping all NSAIDs immediately.

Alternatives to NSAIDs for Pain
You don’t have to suffer to stay safe. There are other ways to manage pain without risking your gut.- Acetaminophen (Tylenol): Safer for your stomach-but don’t exceed 3,000 mg a day. It can harm your liver if you drink alcohol or take it too long.
- Physical therapy: For arthritis, back pain, or joint issues, movement is medicine. A physical therapist can teach you exercises that reduce pain without pills.
- Topical NSAIDs: Gels and patches applied to the skin (like diclofenac gel) deliver pain relief with far less risk to your stomach.
- Heat, ice, massage: Simple, free, and effective for many types of chronic pain.
- Acupuncture or mindfulness: Studies show these can reduce pain perception and decrease reliance on medication.
The Bigger Picture
NSAIDs are everywhere. They’re in medicine cabinets, grocery stores, and vending machines. We treat them like candy-harmless, quick, and safe. But they’re powerful drugs with serious side effects that most people don’t know about.Doctors aren’t always the ones to warn you. You have to be your own advocate. If you’ve been taking NSAIDs for more than a few weeks, ask: Is this still necessary? Am I at risk? Could there be a safer way?
The goal isn’t to scare you off all pain relief. It’s to make sure you’re not trading one problem for a far worse one. Your gut doesn’t scream before it breaks. But if you listen-really listen-to your body and your meds, you can avoid the bleed before it starts.
Can I take aspirin daily if I’m on other NSAIDs?
No. Combining daily aspirin with any other NSAID-ibuprofen, naproxen, etc.-doubles your risk of gastrointestinal bleeding. Even low-dose aspirin (81 mg) for heart protection becomes dangerous when mixed with other painkillers. If you need both, talk to your doctor about switching to a safer pain reliever like acetaminophen or using a proton pump inhibitor for protection.
Are COX-2 inhibitors like Celebrex safer for the stomach?
They’re less likely to cause upper GI ulcers than traditional NSAIDs-but only if you’re not taking aspirin. If you’re on daily aspirin, COX-2 inhibitors offer no extra protection. Your bleeding risk stays just as high. They’re not a magic solution, and they still carry heart risks. Always weigh the full picture with your doctor.
How do I know if I’m bleeding internally from NSAIDs?
You might not feel anything. The most common sign is unexplained anemia-low iron or low hemoglobin on a blood test. Other signs include fatigue, dizziness, pale skin, or black, sticky stools. If you’ve been taking NSAIDs for months and feel unusually tired, ask your doctor to check your blood. Don’t wait for vomiting or bright red blood-that’s often too late.
Is it safe to take NSAIDs occasionally for a headache?
Yes, if it’s rare-once or twice a month, at the lowest effective dose. The danger comes from daily or near-daily use. Occasional use in healthy adults under 50 carries very low risk. But if you’re over 60, have a history of ulcers, or take blood thinners, even occasional use can be risky. Always check with your doctor if you’re unsure.
Can I stop NSAIDs cold turkey if I’m worried about bleeding?
If you’re taking NSAIDs for chronic pain like arthritis, stopping suddenly might cause a flare-up. Don’t quit without talking to your doctor. They can help you taper off safely and suggest alternatives. But if you’re experiencing signs of bleeding-black stools, dizziness, extreme fatigue-stop immediately and seek medical help.
Do I need an endoscopy if I take NSAIDs regularly?
Not routinely-but if you’re over 50, have risk factors like a past ulcer, H. pylori, or are on multiple medications, your doctor may recommend one. Blood tests for anemia are usually the first step. If your hemoglobin is low and no other cause is found, an endoscopy can confirm if NSAIDs are damaging your gut lining.

