When a pharmaceutical company changes even a small part of how a drug is made, it’s not just an internal decision. It’s a regulatory event. The FDA, EMA, Health Canada, and other agencies don’t let manufacturers tweak equipment, switch suppliers, or move production lines without strict rules. Why? Because a tiny change in the process can affect the safety, strength, or purity of a medicine. One wrong move - like replacing a mixer without approval - could lead to a recall, a warning letter, or even a shutdown. This isn’t theoretical. In 2023, the FDA issued four warning letters just for misclassified equipment changes. If you work in pharma manufacturing, you need to know exactly when to notify regulators - and when to wait for approval before making a move.
What Counts as a Manufacturing Change?
A manufacturing change isn’t just about big equipment swaps. It includes anything that touches how the drug is made: switching raw material suppliers, changing the location of a step in the process, updating software that controls a machine, or even replacing a filter with a different brand. The key question regulators ask is: Could this change affect the product’s identity, strength, quality, purity, or potency? If the answer is yes, you’re in regulated territory.For example, replacing a tablet press with the exact same model from the same manufacturer? That’s often a moderate change. But switching from a rotary press to a high-shear mixer? That’s a major change. Even something as small as changing the water source used to clean equipment can trigger a notification if it impacts microbial levels in the final product.
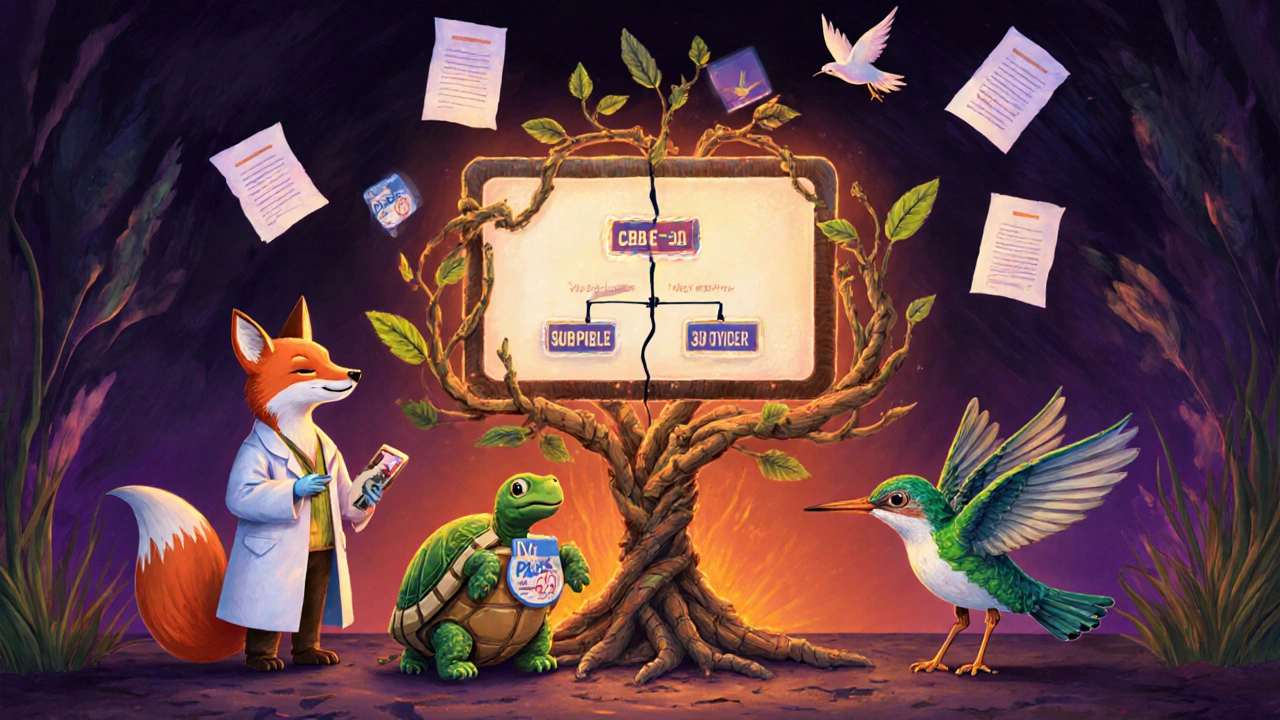
The FDA’s Three-Tier System
The U.S. FDA uses a clear, risk-based system to classify manufacturing changes. There are three categories:- Prior Approval Supplement (PAS) - for major changes. You must get FDA approval before making the change or shipping any product made with it. Examples: changing the synthetic route of an active ingredient, moving critical production to a new facility, or altering a sterilization process that affects sterility assurance.
- Changes Being Effected in 30 Days (CBE-30) - for moderate changes. You can implement the change after submitting the supplement, but you must wait 30 days before distributing the product. This is common for equipment swaps where the new device has the same design and operating principles - like replacing a filling machine with an identical model from the same vendor.
- Annual Report - for minor changes. These are low-risk adjustments, like moving a packaging line within the same building or updating a non-critical label. You don’t need to notify the FDA ahead of time. Just document it and include it in your next annual report.
Getting this wrong is expensive. In 2019, Apotex got a warning letter for classifying a major change as moderate. The FDA found they’d changed the drying method for a critical API without approval - and shipped over 1 million units. That’s not just a compliance issue. It’s a patient safety risk.
How Other Regulators Compare
The FDA isn’t the only player. The European Medicines Agency (EMA) uses a different system:- Type IA - minor changes. You can implement them immediately and notify within 12 months.
- Type IB - moderate changes. You must get approval before implementation, but the review is faster than for Type II.
- Type II - major changes. Full review required before any change is made.
Health Canada mirrors the FDA’s structure with Level I (prior approval), Level II (notify and wait), and Level III (annual report). The big difference? EMA allows some changes to be implemented before notification (Type IA), while the FDA doesn’t. That’s a key flexibility that some manufacturers prefer.
For biologics - like vaccines or gene therapies - the rules are even tighter. The FDA’s 2021 guidance specifically says that even small changes to cell culture conditions or purification steps often require a PAS because the product is so sensitive. A change that’s minor in a tablet might be major in a monoclonal antibody.
How to Classify a Change Correctly
There’s no checklist that works for every situation. But there’s a process:- Identify the change. What exactly is being altered? Equipment? Process? Location? Supplier?
- Map it to quality attributes. Which Critical Quality Attributes (CQAs) could be affected? Purity? Potency? Dissolution rate? Particle size?
- Assess the risk. Use tools like FMEA (Failure Modes and Effects Analysis). Ask: How likely is failure? How severe is the impact?
- Review the guidance. FDA’s 2021 biologics guidance has a table listing over 50 common changes and their recommended categories. Use it as a starting point.
- Consult early. If you’re unsure, reach out to the FDA. Their 2021 guidance says: “If FDA disagrees with your classification, it may delay approval.” Better to ask now than get a warning letter later.
One senior regulatory affairs specialist on Reddit shared that classifying a tablet press replacement took 37 hours of team time because the API’s particle size specs were ambiguous. That’s not inefficiency - that’s due diligence.
What Documentation Do You Need?
You can’t just say “we think this is minor.” You have to prove it. Required documentation includes:- Facility diagrams showing new or modified equipment locations
- Process validation reports comparing old and new methods
- Comparative batch data from at least three consecutive batches made with the new process
- Stability data showing the product still meets specs after the change
- Risk assessment report (FMEA or equivalent)
For a CBE-30 submission, you need enough data to show the change won’t harm quality. For a PAS, you need full comparability studies - often including bioequivalence testing for oral products.
Who’s Involved in the Process?
This isn’t a job for one person. A cross-functional team is essential:- Quality Assurance - owns the change control system and ensures documentation is complete.
- Manufacturing - knows the equipment, process limits, and operational realities.
- Regulatory Affairs - interprets the rules and files the correct submission.
- Validation - runs tests to prove the new process works as intended.
- Supply Chain - flags supplier changes and ensures material traceability.
According to a 2021 PDA study, moderate changes require about 120 hours of combined team effort. For a PAS, it can be 500+ hours. That’s why small companies struggle - they don’t have the bandwidth.
What Happens If You Get It Wrong?
The consequences are real:- Warning letters - public, posted on the FDA website. Damages reputation.
- Product recalls - costly and disruptive. In 2022, 22% of all FDA warning letters cited manufacturing change violations.
- Import alerts - your product gets blocked at the border.
- Consent decrees - court-enforced oversight. Could shut down production for months or years.
In Q2 2023, Lupin Pharmaceuticals got a warning letter for replacing a lyophilizer (freeze-dryer) without a PAS. The FDA found the new unit had different drying profiles - potentially altering product stability. That’s not a technical glitch. That’s a failure in change management.
Industry Trends and Future Changes
The regulatory landscape is evolving. The ICH Q12 guideline, adopted in 2020, is pushing for more flexibility in post-approval changes. It encourages companies to use lifecycle management and real-time data to reduce regulatory burden.More companies are using real-time monitoring systems - like sensors that track temperature, pressure, and moisture during production - to prove consistency. By 2025, McKinsey predicts 40% of new change submissions will include this kind of data. That could mean fewer PAS submissions for equipment changes if you can prove the process stays in control.
Continuous manufacturing - where drugs are made in one long, uninterrupted flow - is growing. But it’s tricky. Because every step is linked, even a small equipment change can ripple through the whole process. That’s why most continuous manufacturing changes still require PAS submissions.
Meanwhile, the EMA introduced faster review paths for Type IB changes in 2023, cutting approval times from 60 to 30 days for certain equipment upgrades. The FDA is expected to follow suit with its 2023 draft guidance on quality risk management.
Final Takeaway
Manufacturing changes aren’t about compliance for compliance’s sake. They’re about protecting patients. Every change, no matter how small, has the potential to impact medicine quality. The system isn’t perfect - it’s complex, time-consuming, and sometimes ambiguous. But it’s designed to prevent harm.If you’re unsure whether a change is major or minor, err on the side of caution. Document everything. Involve the right people. And when in doubt, ask the regulator. It’s better to wait 30 days for approval than to risk a recall, a warning letter, or worse - a patient getting a bad batch of medicine.
What’s the difference between a PAS and a CBE-30?
A PAS (Prior Approval Supplement) requires FDA approval before you can make the change or ship any product made with it. It’s used for major changes that could affect safety or effectiveness, like switching the synthesis method for a drug’s active ingredient. A CBE-30 (Changes Being Effected in 30 Days) lets you implement the change after submitting the notice, but you must wait 30 days before distributing the product. It’s for moderate changes, like replacing a mixer with an identical model from the same manufacturer. The key difference is timing: PAS = approval first. CBE-30 = notify then wait.
Can I make a manufacturing change without telling the FDA?
Only for minor changes that go in your annual report. These are low-risk adjustments - like moving a labeling machine within the same facility or changing a non-critical supplier. If the change affects the drug’s identity, strength, purity, or potency, you must notify the FDA before or during implementation. Making a major change without approval is a serious violation and can lead to recalls or shutdowns.
How do I know if equipment is "equivalent"?
The FDA defines "equivalent" equipment as having the same principle of operation, same critical dimensions, and same material of construction. For example, replacing a tablet press with another model from the same vendor that has identical compression force settings, punch size, and stainless steel contact surfaces would typically qualify. If you’re using a different brand, even with similar specs, you’ll need to prove comparability through testing - and may need a CBE-30 or even a PAS.
What’s the biggest mistake companies make with manufacturing changes?
The most common mistake is assuming a change is minor because it’s "just a replacement." Companies often overlook how equipment changes can affect critical process parameters - like mixing time, heat transfer, or particle size distribution. Even if the new machine looks identical, subtle differences in motor speed or vibration can alter the product. Always test and document. Don’t rely on appearances.
Do small companies have an easier time with change approvals?
No - they have a harder time. Small companies often lack dedicated regulatory staff, validation teams, or resources to run full comparability studies. While the FDA treats all companies the same under the law, smaller firms are more likely to misclassify changes due to limited expertise. FDA inspection data shows only 63% of small and mid-sized companies fully comply with change control requirements, compared to 98% of large pharma firms. Training and external consultants are often necessary to close the gap.
12 Comments
Write a comment