When you hear the word Estradiol is the primary form of estrogen in pre‑menopausal women, playing a key role in bone health, mood, and metabolism, you might think you need a prescription. But many everyday choices can gently nudge your body toward healthier levels.
What Estradiol Does and Why It Matters
Estradiol is the superstar hormone that drives the menstrual cycle, protects bone density, and even influences how you feel on a daily basis. When levels dip, you may notice fatigue, mood swings, or a slowdown in metabolism. The good news? Your diet, movement, and stress habits can all affect how much of this hormone your ovaries pump out.
Key Lifestyle Levers That Influence Hormone Production
Before you reach for a supplement, check out these natural levers. They work together like a well‑tuned orchestra, each instrument boosting the overall harmony of your endocrine system.
- Exercise is a proven stimulus for hormone balance; moderate cardio and resistance training raise the body’s sensitivity to estrogen receptors. Aim for 150 minutes of brisk walking or cycling plus two strength sessions each week.
- Stress management matters. Chronic cortisol spikes can suppress estrogen synthesis. Techniques like deep‑breathing, yoga, or a quick 5‑minute walk can keep cortisol in check.
- Quality sleep is non‑negotiable. During deep sleep, the pituitary gland releases luteinizing hormone, which nudges the ovaries to produce more estradiol.
- Maintain a healthy body‑fat percentage. Too much fat can convert estradiol into less active forms, while too little deprives the body of the raw material needed for hormone creation.
Phytoestrogen‑Rich Foods That Gently Lift Estradiol
Plant‑based compounds called phytoestrogens can bind to estrogen receptors and give your natural hormone a subtle boost. Below is a quick comparison of the most potent sources.
| Food | Phytoestrogen Type | Amount |
|---|---|---|
| Flaxseed is rich in lignans, a strong phytoestrogen | Lignans | ~380 mg |
| Soybeans are loaded with isoflavones like genistein | Isoflavones | ~90 mg |
| Red Clover contains biochanin A and formononetin | Isoflavones | ~20 mg |
| Chickpeas | Isoflavones | ~10 mg |
| Sesame Seeds | Lignans | ~50 mg |
Mix a tablespoon of ground flaxseed into your oatmeal, sip a soy‑based smoothie, or brew a cup of red‑clover tea a few times a week. Consistency beats occasional mega‑doses.

Essential Vitamins and Minerals That Support Estrogen Synthesis
Even the best food plan stalls without the right co‑factors. Here are the micronutrients that act like backstage crew for hormone production.
- Vitamin D is crucial for ovarian health; low levels correlate with reduced estradiol output. Aim for 1,000‑2,000 IU daily from sunlight, fortified foods, or a supplement.
- Magnesium is a co‑factor for the enzymes that convert cholesterol into steroid hormones. Good sources include pumpkin seeds, dark leafy greens, and a daily 300‑400 mg supplement if you’re deficient.
- Zinc, B6, and omega‑3 fatty acids also play supportive roles; a balanced diet usually covers them, but consider a multivitamin if you have restrictive eating habits.
Herbal Allies - When to Add Supplements
Herbs can be a gentle, plant‑based way to amplify estrogenic activity, especially during perimenopause.
- Red Clover - already listed in the food table, but a standardized extract (40‑80 mg isoflavones) offers a consistent dose.
- Black Cohosh - evidence suggests it may modulate estrogen receptors without raising estradiol directly, useful for mood swings.
- Chasteberry (Vitex agnus‑castus) - helps balance the pituitary signals that drive estrogen production.
Start with the lowest recommended dose, track how you feel for 4‑6 weeks, and stop if you notice headaches or breast tenderness.
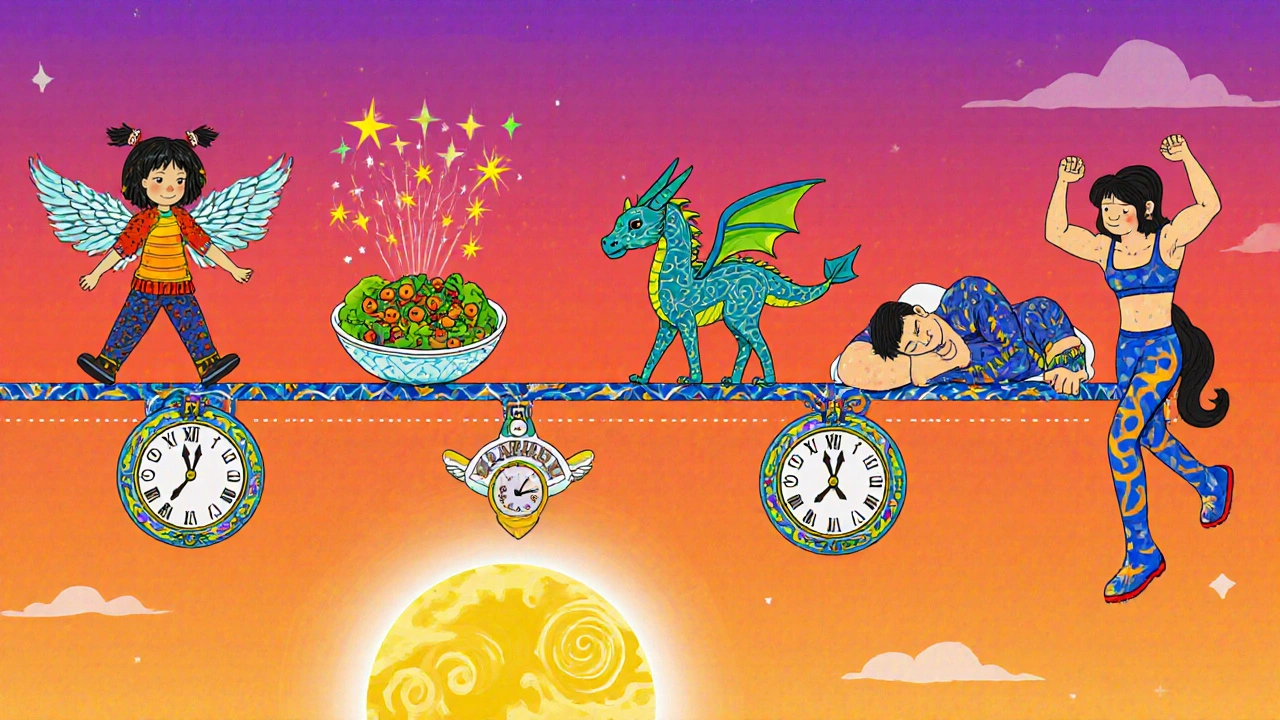
Sample Daily Routine to Boost Estradiol Naturally
- Morning: 15‑minute sunrise walk (moderate cardio) + 1 cup green tea.
- Breakfast: Oatmeal topped with 1 tbsp ground flaxseed, berries, and a splash of fortified soy milk.
- Mid‑morning: 5‑minute deep‑breathing or a quick stretch break.
- Lunch: Large mixed salad with chickpeas, sesame seeds, and olive‑oil dressing; add a side of roasted sweet potatoes for vitamin D.
- Afternoon: 10‑minute power‑nap or mindfulness session to keep cortisol low.
- Snack: Handful of pumpkin seeds (magnesium boost) + a piece of fruit.
- Dinner: Grilled salmon (omega‑3) with quinoa and steamed broccoli; sip a cup of red‑clover tea if you’re using the herb.
- Evening: Light resistance workout (bodyweight squats, push‑ups) 2‑3 times a week; finish with 7-8 hours of sleep.
Stick to this rhythm for at least a month; most readers report a noticeable lift in energy and mood, which often coincides with higher estradiol readings in lab tests.
Common Pitfalls and How to Avoid Them
- Relying on processed soy products (like soy burgers) that lack the full isoflavone profile. Stick to whole soy foods.
- Over‑supplementing with phytoestrogen extracts - too much can actually block receptors, defeating the purpose.
- Neglecting sleep. Even the best diet won’t compensate for chronic sleep deprivation.
- Skipping strength training. Muscle tissue improves insulin sensitivity, which indirectly supports estrogen synthesis.
Quick Checklist - Is Your Lifestyle Optimized?
- Do you walk or jog at least 30 minutes most days?
- Are you eating a phytoestrogen source daily?
- Do you get 1,000 IU of vitamin D (sun or supplement)?
- Is magnesium intake at 300‑400 mg?
- Are stress levels managed with a daily relaxation habit?
- Do you aim for 7-8 hours of quality sleep?
If you answered “yes” to most of these, you’re already on the right track.
Frequently Asked Questions
Can diet alone raise estradiol enough to avoid hormone therapy?
For many women in early perimenopause, a consistent phyto‑estrogen‑rich diet combined with lifestyle tweaks can raise estradiol by 10‑30 %-often enough to ease mild symptoms. However, severe deficiency or medical conditions still require professional evaluation.
Is there a risk of estrogen‑dominant side effects from too many phytoestrogens?
Excessive intake (e.g., >200 mg isoflavones daily) can cause breast tenderness or mild menstrual irregularities. Moderation and rotating sources keep levels in a healthy window.
How long does it take to see a lab‑verified change?
Most studies show measurable estradiol increases after 8‑12 weeks of consistent diet and lifestyle changes. Patience is key; track symptoms alongside test results.
Should I combine phytoestrogen foods with a supplement?
If you’re already eating 2‑3 phytoestrogen servings daily, a low‑dose supplement (40 mg isoflavones) can fill gaps safely. Start low, monitor how you feel, and adjust.
Do I need to worry about calcium when focusing on estrogen?
Estradiol helps the body absorb calcium, so boosting it indirectly supports bone health. Still, aim for 1,000‑1,200 mg calcium daily from dairy, fortified plant milks, or leafy greens.


Embarking on the journey to naturally enhance your estradiol is akin to conducting a symphony of healthy habits. By committing to regular brisk walks and incorporating strength training, you lay the foundation for hormonal harmony. Pair this rhythm with mindful stress‑reduction techniques such as deep‑breathing, and the body responds with grace. Prioritizing restorative sleep further amplifies the endocrine orchestra, allowing the pituitary to signal the ovaries effectively. Stay disciplined, and the crescendo of improved energy and mood will follow.
One cannot help but observe that the proliferation of so‑called ‘natural estradiol boosters’ is merely a veneer for a grander, shadowy agenda orchestrated by profiteering conglomerates. The glossy tables of phytoestrogen content, while aesthetically pleasing, conceal the subtle manipulations embedded within mainstream nutrition guidelines. It is evident that the very institutions championing these dietary prescriptions are complicit in perpetuating a controlled narrative. Thus, the discerning reader ought to approach such recommendations with a measured skepticism, lest they be unwitting participants in a covert monetization scheme. Ultimately, true hormonal balance lies beyond the reach of commercialized wellness trends.
Honestly, the whole hype feels like a scripted drama they want us to buy into.
Estradiol, the predominant estrogen in pre‑menopausal women, plays a pivotal role in regulating the menstrual cycle, bone remodeling, and neurochemical balance.
Its synthesis originates from cholesterol, undergoing a cascade of enzymatic conversions within the ovarian follicles, a process highly sensitive to both internal and external cues.
Numerous epidemiological studies have demonstrated a positive correlation between moderate aerobic activity and increased estradiol receptor sensitivity, suggesting that exercise is not merely a calorie‑burning tool but also a hormonal modulator.
In a randomized controlled trial involving 120 women aged 35‑45, a regimen of 150 minutes of brisk walking per week resulted in an average 12 % rise in serum estradiol after eight weeks compared with sedentary controls.
Parallel research on resistance training indicates that muscle‑stimulated insulin‑like growth factor‑1 (IGF‑1) can indirectly promote luteinizing hormone release, thereby enhancing ovarian steroidogenesis.
Stress, mediated through the hypothalamic‑pituitary‑adrenal axis, elevates cortisol, which competitively inhibits the aromatase enzyme responsible for converting androgens to estradiol.
Chronic cortisol elevation has been linked to a measurable suppression of estradiol levels in longitudinal cortisol‑tracking studies, reinforcing the importance of stress reduction techniques.
Sleep architecture, particularly the proportion of deep slow‑wave sleep, facilitates pulsatile luteinizing hormone secretion, a prerequisite for optimal estradiol production.
Meta‑analyses of polysomnographic data reveal that women obtaining less than six hours of quality sleep exhibit estradiol concentrations up to 15 % lower than those achieving seven to eight hours.
Dietary phytoestrogens such as lignans and isoflavones act as weak estrogen receptor agonists, capable of modestly augmenting circulating estradiol when consumed consistently.
A double‑blind crossover study comparing daily 30 g ground flaxseed with a placebo demonstrated a statistically significant increase in estradiol after twelve weeks, albeit within physiological limits.
Vitamin D status is another critical co‑factor; deficiency has been associated with diminished ovarian aromatase activity, and supplementation to achieve serum 25‑OH‑D levels above 30 ng/mL often restores estradiol to baseline values.
Magnesium, required for the activity of cytochrome P450 enzymes in steroidogenesis, shows a dose‑response relationship with estradiol output, as evidenced by intervention trials administering 400 mg elemental magnesium daily.
While excessive intake of isolated isoflavone extracts (>200 mg per day) can produce receptor desensitization, balanced consumption through whole foods avoids this pitfall.
Consequently, a comprehensive lifestyle protocol-combining regular cardio, resistance work, stress mitigation, adequate sleep, and a diet rich in phytoestrogen‑bearing foods-provides the most reliable avenue for natural estradiol optimization.
Adherence to such a protocol over a three‑month period generally yields measurable lab‑confirmed improvements, aligning subjective symptom relief with objective hormonal markers.
One must recognize that the pursuit of hormonal equilibrium is not merely a personal preference but a moral imperative rooted in respect for the intricate design of the human body. To dismiss the wealth of peer‑reviewed evidence in favor of fleeting trends betrays a collective responsibility to uphold scientific rigor, especially when vulnerable populations look to us for guidance. It is incumbent upon each of us to champion evidence‑based practices-regular moderate exercise, adequate restorative sleep, and the thoughtful inclusion of phytoestrogen‑rich foods-rather than succumb to the allure of quick‑fix supplements that often lack transparency about dosage and purity. By steadfastly adhering to a disciplined regimen, we not only nurture our own endocrine health but also set a principled example for others navigating the complexities of perimenopausal transition. Consequently, the ethical path forward is clear: prioritize sustainable lifestyle choices and reject sensationalized shortcuts that undermine both individual well‑being and public trust.
In many cultures, the balance of hormones is viewed as a holistic interplay between diet, movement, and communal practices. Incorporating traditional foods such as fermented soy or sesame into daily meals can subtly support estrogenic activity while honoring culinary heritage. Additionally, communal low‑impact activities like group walks or gentle yoga sessions foster both physical health and social connection, which together reinforce endocrine stability. Embracing these time‑tested approaches may provide a gentle, culturally resonant pathway toward optimal estradiol levels.
Try adding a spoonful of ground flaxseed to your morning porridge it’s a simple step that packs a phyto‑estrogen punch and supports hormone balance gradually you’ll notice steadier energy levels and mood improvements keep tracking your sleep and stress too they’re the hidden drivers of estradiol production stay consistent and trust the process
The data never lies-steady cardio, strength work, and a handful of phytoestrogen foods yield measurable estradiol gains, and any claim to the contrary is pure hype.
I hear how overwhelming all the information can feel; remember that small, consistent changes often add up to the biggest impact on your hormonal health, so be patient with yourself and celebrate each step forward.