Therapy isn’t just about the copay - here’s what else you’re really paying
You show up for your therapy session, swipe your card, and pay $30. That’s it, right? Maybe. But that $30 is just one piece of a much bigger financial puzzle. If you’re relying on insurance to cover therapy, you might be surprised to find out your total cost could be hundreds - even thousands - of dollars more than what you pay at the door.
Most people assume their copay is the full cost of therapy. It’s not. Insurance plans are built with layers: deductibles, coinsurance, out-of-pocket maximums, network rules, and sometimes even separate mental health deductibles. Skip these details, and you could end up with a bill you never saw coming.
Know your plan type - it changes everything
Not all insurance plans work the same way. There are three main structures, and each affects your total therapy cost differently.
- Copay plans: You pay a fixed amount per session - say $30 - no matter what the actual session costs. Sounds simple, right? But only if you’ve already met your deductible. If you haven’t, you might be paying the full price until you hit that number.
- Deductible plans: You pay 100% of the session cost until you’ve spent a set amount (your deductible) in a year. That could be $1,500, $3,000, or more. If your therapist charges $125 per session, you’d pay $125 x 12 = $1,500 just to get to the point where your copay kicks in.
- Coinsurance plans: After you meet your deductible, you pay a percentage of each session. Common rates are 20% or 40%. So if your session is $125 and your coinsurance is 20%, you pay $25. But if your session is $227 (like in North Dakota), you’re paying $45.40 - and that adds up fast.
Thriveworks’ 2024 study found that the average therapy session without insurance costs $143.26. With insurance, your out-of-pocket cost depends entirely on which of these structures you’re under. Your copay might be $30 - but if you’re still in deductible mode, you’re really paying $143.26. And if you’re on coinsurance, you might pay $28 to $57 per session after meeting your deductible.
Out-of-network therapy can cost 2x more
If you see a therapist who isn’t in your insurance network, you’re entering a different financial world. Out-of-network providers don’t have pre-negotiated rates with your insurer. That means you pay the full fee upfront - and then submit a claim for partial reimbursement.
Alma’s 2023 analysis shows that out-of-network patients typically pay 40-50% of the session cost after meeting their deductible. In-network? That’s usually 20-30%. So if you’re paying $125 per session in-network with 20% coinsurance, you pay $25. Out-of-network? You might pay $60-$70 per session after reimbursement.
And here’s the kicker: out-of-network rates vary wildly by location. A $143 session in Arizona might be $227 in North Dakota. That’s a $84 difference per session - multiplied by 20 sessions - that’s $1,680 more in one year. Geography matters more than you think.
Your deductible isn’t just for therapy
Most people think their deductible only applies to mental health services. It doesn’t. Your deductible is usually a total annual amount you must pay across all covered medical services - doctor visits, lab tests, prescriptions, physical therapy, and therapy.
That means if you broke your ankle in January and paid $1,200 in medical bills, and your deductible is $1,500, you only have $300 left to pay before therapy copays kick in. But if you have a separate mental health deductible (some plans do), then your $1,200 medical bill doesn’t count toward your therapy deductible at all.
Shasta Health’s 2023 report found that nearly 40% of patients didn’t realize their copay obligations until after they started therapy. Why? Because they assumed their deductible was only for therapy. It wasn’t. And now they’re stuck with a $1,200 bill they didn’t budget for.
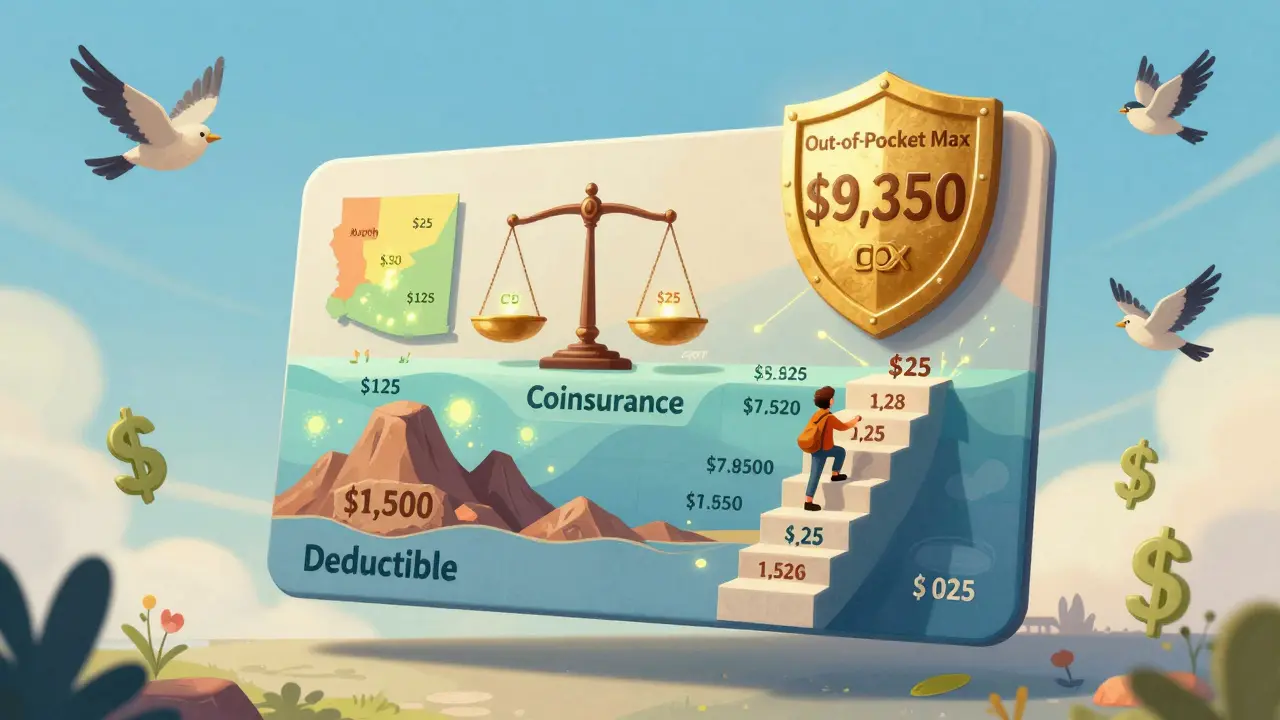
Out-of-pocket maximums are your safety net - but only if you know they exist
There’s a limit to how much you’ll ever pay in a year for covered services. That’s your out-of-pocket maximum. In 2024, the federal cap for individual plans is $9,350. For families, it’s $18,700.
Once you hit that number, your insurance pays 100% of covered therapy costs for the rest of the year. But here’s the catch: you have to actually reach it. If you’re on a coinsurance plan and need 30 sessions at $125 each, your total cost could be $3,750 - way below the cap. But if you need 60 sessions - common for complex trauma or chronic depression - you might hit $7,500 in therapy alone, not counting other medical bills.
Let’s say you have a $3,000 deductible and 20% coinsurance. Your therapist charges $125/session. You need 40 sessions. Here’s how it breaks down:
- First 24 sessions: $125 x 24 = $3,000 (meets deductible)
- Next 16 sessions: 20% of $125 = $25 x 16 = $400
- Total: $3,400
That’s still under the out-of-pocket max. But if your therapist charges $200/session? Now you’re paying $4,800 for 24 sessions - and you’re already halfway to your max. The numbers change fast when prices rise.
Medicare and Medicaid are different - here’s how
If you’re on Medicare, you pay 20% of the Medicare-approved amount after meeting your Part B deductible. Thriveworks found the average patient pays $28.65 per session. That’s lower than most private insurance copays - but you still pay it. And if you don’t have a Medigap Plan G, you’re on the hook for the rest.
Medicaid is usually more generous. Most Medicaid plans have little to no copay for therapy. But availability varies by state. In some places, you’ll need to use specific providers. In others, you can choose freely. Check your state’s Medicaid portal - don’t assume.
Sliding scale and low-cost options aren’t just for the uninsured
You don’t need to be broke to qualify for lower-cost therapy. Around 42% of private practice therapists offer sliding scale fees based on income - not insurance status. That means even if you have insurance with a high deductible, you might still qualify for a reduced rate if your income is below a certain level.
Platforms like Open Path Collective connect people with therapists who charge $40-$70 per session, regardless of insurance. University training clinics, staffed by supervised grad students, often charge 50-70% less than market rates. These aren’t last-resort options - they’re smart financial tools.
And here’s the trick: you can use these even if you have insurance. Some people use sliding scale therapy until they meet their deductible, then switch to in-network therapy. Others use it for long-term maintenance after insurance coverage runs out.

Build a real budget - not a guess
Here’s how to calculate your total therapy cost step by step:
- Find your plan type - copay, deductible, or coinsurance? Call your insurer or check your portal.
- Check your deductible - how much have you paid so far this year? How much is left?
- Confirm your therapist’s rate - ask if they’re in-network. If not, ask what their fee is and what your insurer allows.
- Estimate your session count - most people need 12-16 sessions for improvement. For complex issues, expect 15-20 or more.
- Calculate Phase 1 (pre-deductible) - if you haven’t met your deductible, multiply your session cost by the number of sessions until you hit it.
- Calculate Phase 2 (post-deductible) - multiply your copay or coinsurance by remaining sessions.
- Add your premiums - don’t forget your monthly insurance payment. Multiply by 12.
- Check your out-of-pocket max - if your projected costs are close to it, you’ll pay less than you think.
Example: You have a $1,500 deductible, $40 copay, and 20 sessions at $125 each. You’ve paid $500 toward your deductible already.
- Phase 1: You need $1,000 more to meet deductible → 8 sessions x $125 = $1,000
- Phase 2: 12 sessions left x $40 = $480
- Total therapy cost: $1,480
- Plus $300/month premium x 12 = $3,600
- Total annual cost: $5,080
That’s not $30 per session. That’s over $5,000 a year. And you’re not even counting transportation, missed work, or medication.
Tools that actually help
You don’t have to do this alone. Use these:
- Your insurer’s online portal - it shows your deductible progress and copay amounts.
- Alma’s free Cost Estimator Tool - enter your plan, therapist, and session count. It breaks down what you’ll pay now vs. later.
- Rula’s cost estimator - reports average insurance-paid session costs around $15, but your number will vary.
- GoodRx - check medication costs if you’re on antidepressants or anti-anxiety meds. Those add up too.
Don’t wait until your bill arrives to understand your costs. Call your insurer. Ask for a benefits summary. Print it out. Put it in your wallet.
Final tip: Time your therapy smartly
If you’re planning long-term therapy, consider starting it in January. That gives you the full year to meet your deductible. If you start in October, you might pay full price for 3 months, then hit your deductible in January - but your insurance resets. You’ll pay full price again next year.
Some people time their therapy to align with other medical needs. Got a physical therapy appointment in March? Add a therapy session that same week. Every covered service counts toward your deductible. Stack them.
Therapy is worth it - but only if you know what you’re paying
Therapy changes lives. But financial stress can make it feel impossible. The good news? You have more control than you think. By understanding your plan, tracking your spending, and using low-cost options, you can make therapy affordable - even if your copay is just the tip of the iceberg.
Don’t let surprise bills stop you from getting help. Know your numbers. Plan ahead. And don’t be afraid to ask: "What will this really cost me?"
Is my copay the only thing I pay for therapy?
No. Your copay is only part of the cost. If you haven’t met your deductible, you may pay the full session fee. After meeting your deductible, you might pay coinsurance (a percentage) instead of a fixed copay. You also pay monthly premiums, and if you’re out-of-network, you could pay more upfront with partial reimbursement later.
How do I find out what my deductible is?
Call your insurance company’s member services number (on the back of your card) or log into your online portal. Look for "medical deductible," "mental health deductible," or "out-of-pocket costs." Ask: "How much have I paid toward my deductible this year?" and "What’s my out-of-pocket maximum?"
Can I use therapy from a sliding scale provider even if I have insurance?
Yes. Many people use sliding scale providers to reduce costs before meeting their deductible, or after they’ve maxed out their insurance benefits. Some use it for long-term maintenance. You don’t need to be uninsured to qualify - income is the main factor.
Why does therapy cost more in some states?
Therapy prices vary by region due to cost of living, provider supply, and demand. For example, sessions in New York average $176, while in North Dakota, they’re $227. Insurance allowed amounts also vary by location, so even with the same coinsurance rate, your out-of-pocket cost can be much higher in expensive areas.
What happens if I go over my out-of-pocket maximum?
Once you hit your out-of-pocket maximum for the year, your insurance covers 100% of all in-network covered services - including therapy - for the rest of the year. That’s the cap. But you must stay in-network. Out-of-network services may not count toward this limit, depending on your plan.
Do prescription meds for mental health count toward my therapy deductible?
Yes. Any covered medical service - including prescriptions, doctor visits, lab work, and therapy - counts toward your overall medical deductible. So if you’re paying for antidepressants, those bills help you reach your deductible faster, lowering your therapy costs later.
How many therapy sessions do I really need?
Most people see improvement after 12-16 sessions. For complex issues like PTSD or chronic depression, 15-20 sessions are common. Some need ongoing support. Don’t assume you’ll need just 6 sessions. Plan for 12-20 to avoid financial surprises.
Can I switch therapists if my costs are too high?
Yes. If your current therapist is out-of-network or charges too much, you can switch to an in-network provider, a sliding scale therapist, or a training clinic. Your mental health matters - but so does your budget. Finding a lower-cost option doesn’t mean lower quality.


14 Comments
Write a comment