Every year, tens of thousands of people end up in the hospital-not because their condition got worse, but because something they took to get better made something else they were taking dangerous. This isn’t rare. It’s happening right now, to people you know. Drug interactions are one of the most common, preventable causes of medication harm. And most people have no idea they’re at risk.
What Exactly Is a Drug Interaction?
A drug interaction happens when something changes how a medication works in your body. It could be another pill, a supplement, grapefruit juice, or even a health condition you already have. These aren’t just theoretical risks. They’re real, measurable, and often deadly. There are three main types:- Drug-drug interactions: When two or more medications affect each other. For example, taking warfarin (a blood thinner) with certain antibiotics can make your blood too thin, leading to uncontrolled bleeding.
- Drug-food/drink interactions: What you eat or drink can change how your body absorbs or breaks down a drug. Grapefruit juice, for instance, can cause statins like simvastatin to build up to toxic levels in your blood-sometimes leading to muscle breakdown and kidney failure.
- Drug-condition interactions: Your existing health problems can make a drug unsafe. For example, beta-blockers might be fine for most people with high blood pressure, but they can make asthma symptoms worse by blocking the same receptors asthma meds need to work.
These aren’t minor side effects. They’re pharmacological events that can turn a safe treatment into a life-threatening one.
Why This Isn’t Just a ‘Minor Risk’
Let’s put numbers to it. In the U.S., drug interactions cause about 6.5% of all hospital admissions. That’s over 1.3 million emergency visits and 350,000 hospital stays every year-almost all of them preventable. The annual cost? Around $30 billion. And according to a 2022 study in JAMA Internal Medicine, these interactions contribute to roughly 106,000 deaths annually. One of the most dangerous drugs when it comes to interactions is warfarin. It has more than 600 known interactions. That means if you’re on warfarin, nearly every new medication, supplement, or even a change in your diet could throw your blood clotting off balance. A single antibiotic, a new multivitamin, or a glass of grapefruit juice can send your INR (a blood test that measures clotting time) skyrocketing or crashing. And it’s not just warfarin. Digoxin, levothyroxine, statins, and blood pressure meds all have dozens of known interactions. The FDA requires drug labels to list these-but most patients never read them. And even if they did, the labels often don’t explain the real-world risk clearly.How Interactions Actually Happen in Your Body
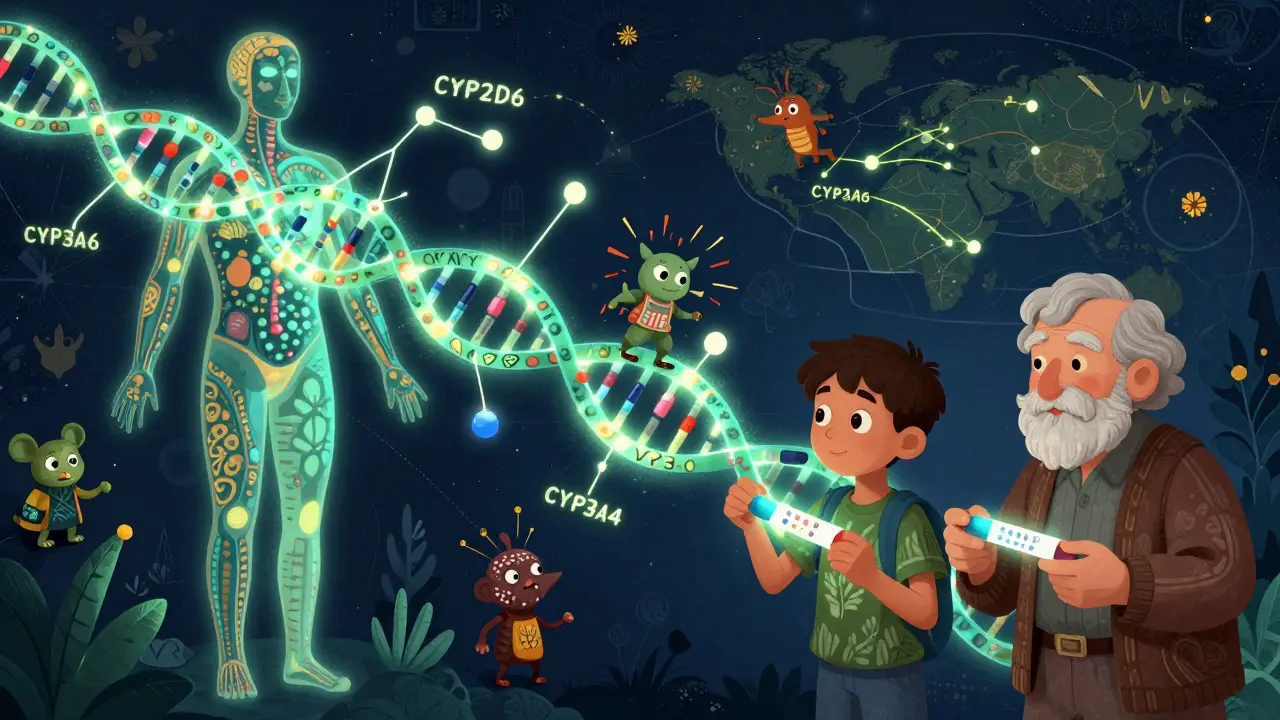
It’s not magic. It’s biology. There are two main ways drugs interfere with each other:- Pharmacokinetic interactions: This is about how your body moves the drug around. The liver uses enzymes-especially CYP3A4-to break down about half of all prescription medications. If another drug blocks or speeds up that enzyme, the medication builds up or gets cleared too fast. Fluconazole (an antifungal) can slow down CYP3A4 so much that simvastatin levels jump by up to 2,000%. That’s not a typo. Two thousand percent. That’s enough to trigger rhabdomyolysis-a condition where muscle tissue breaks down and floods your kidneys with toxic proteins.
- Pharmacodynamic interactions: This is about what the drugs do at their target sites. Two sedatives together? You could fall asleep and not wake up. NSAIDs like ibuprofen with diuretics? They cancel each other out, making your blood pressure meds useless. Beta-blockers with asthma inhalers? They block the same receptors, so your inhaler can’t open your airways.
These aren’t just textbook examples. They’re real stories. One patient on Reddit described taking simvastatin for six months with no issues-then drinking grapefruit juice every morning. Within 48 hours, he was hospitalized with muscle damage. Another woman started a new antidepressant and didn’t tell her doctor she was on a blood pressure med. Her pharmacist caught it before she took the first pill.

Who’s Most at Risk?
It’s not just the elderly. But they’re the most vulnerable. People over 65 take an average of 4.7 prescription drugs daily. And they’re three times more likely to have a dangerous interaction than younger adults. Nearly half of all serious drug interaction events happen in this group-even though they make up only 16% of the population. People with five or more chronic conditions? 68% of them experience at least one significant interaction. And if you’re taking meds metabolized by CYP3A4, CYP2D6, or CYP2C9 enzymes (which cover about 70% of all prescriptions), you’re already in the danger zone. Even if you’re young and healthy, you’re not safe. Taking OTC painkillers with blood thinners? Common. Mixing herbal supplements like St. John’s Wort with antidepressants? Routine. And most people don’t even think of those as “drugs.”What You Can Do to Protect Yourself
You don’t need to be a doctor to prevent these problems. Here’s what actually works:- Keep a complete, up-to-date list of everything you take: prescriptions, over-the-counter meds, vitamins, herbs, and even occasional supplements like melatonin or magnesium. Include the dose and how often you take it.
- Use one pharmacy for all your prescriptions. Pharmacists run drug interaction checks automatically when you fill a new script. If you use multiple pharmacies, you’re bypassing this safety net.
- Ask your pharmacist every time you pick up a new med: “Could this interact with anything else I’m taking?” They’re trained for this. And they’re often the only one who actually checks.
- Don’t assume natural means safe. St. John’s Wort, garlic, ginkgo, and even high-dose vitamin E can interfere with blood thinners, antidepressants, and heart meds. Just because it’s sold in a health food store doesn’t mean it’s harmless.
- Separate your meds from food. If your pill says “take on an empty stomach,” wait at least two hours before eating-especially if you’re on levothyroxine. Calcium, iron, and even coffee can block absorption.
The Beers Criteria-a list of high-risk medications and interactions for older adults-is updated every year by the American Geriatrics Society. If you’re over 65, ask your doctor if any of your meds are on it.
Why Technology Isn’t Enough
Most hospitals and clinics use electronic health records with basic interaction checkers. But here’s the problem: only 42% of them give real-time, severity-ranked alerts. The rest just flag something as “possible.” That’s like having a smoke alarm that only buzzes when the fire’s already in the next room. Even the best databases disagree. A 2022 study found that major drug interaction tools only agreed on the severity of an interaction 63% of the time. That means two pharmacists could look at the same combination and give you two different answers. And here’s the biggest blind spot: clinical trials don’t test for interactions. Only 25% of dangerous interactions are found before a drug hits the market. The rest? They show up after thousands of people are already taking it. Pharmaceutical companies have been accused of underreporting interaction risks in trials. A 2022 study found that 73% of significant interactions were only discovered after the drug was widely used.What’s Changing-and What’s Next
The FDA launched the Drug Interaction Knowledgebase (DIKB) in 2023-a machine-readable database with over 12,000 validated interactions and evidence ratings. That’s a step forward. And AI tools like IBM Watson Health are now analyzing hundreds of millions of clinical notes to find previously unknown interactions. The future? Personalized medicine. Your genes matter. The FDA now includes pharmacogenetic info for over 350 drugs. If you have a variant in the CYP2C9 or CYP2D6 gene, you might process certain drugs 10 times slower than average. By 2026, genetic testing for these enzymes could become standard before prescribing high-risk meds. But until then, the best tool you have is awareness. You are your own best safety net.When to Call Your Doctor
If you notice any of these after starting a new medication:- Sudden dizziness, confusion, or extreme fatigue
- Unexplained bruising or bleeding
- Severe muscle pain or weakness
- Swelling in your legs or ankles
- Heart palpitations or irregular heartbeat
Call your doctor or pharmacist immediately. Don’t wait. Don’t assume it’s “just a side effect.” It might be an interaction.
Medication safety isn’t about avoiding pills. It’s about understanding how they work together. The goal isn’t to stop taking your meds. It’s to take them safely.
Can over-the-counter meds cause dangerous drug interactions?
Yes. Common OTC drugs like ibuprofen, naproxen, antacids, and even cold medicines can interact with prescriptions. For example, ibuprofen can reduce the effectiveness of blood pressure medications and increase bleeding risk if you’re on warfarin. Antacids with aluminum or magnesium can block absorption of thyroid meds and antibiotics. Always check with your pharmacist before taking anything new-even if it’s sold without a prescription.
Is grapefruit juice really that dangerous with statins?
Yes. Grapefruit juice contains compounds that block an enzyme in your gut (CYP3A4) that normally breaks down certain statins like simvastatin, atorvastatin, and lovastatin. This can cause drug levels to spike by 300-600%. That’s enough to cause rhabdomyolysis, a condition where muscle breaks down and can lead to kidney failure. Even one glass a day can be risky. If you take one of these statins, avoid grapefruit entirely. Other citrus fruits like Seville oranges and pomelos have the same effect.
Why do some drug interaction checkers give different results?
Because they use different databases and severity ratings. Professional tools like Lexicomp have over 55,000 interactions with detailed clinical guidance. Consumer tools like WebMD cover about 25,000 and often simplify risk levels. A 2022 study found that major databases agreed on interaction severity in only 63% of cases. Always cross-check with your pharmacist-they have access to the most accurate, up-to-date systems.
Can herbal supplements interact with my prescriptions?
Absolutely. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and HIV meds. Garlic and ginkgo can increase bleeding risk with blood thinners. Coenzyme Q10 may reduce warfarin’s effect. Even vitamin E and fish oil can thin your blood. Many people think “natural” means “safe,” but herbs are potent chemicals. Always tell your doctor and pharmacist exactly what supplements you take-no exceptions.
What should I do if I think I’m having a drug interaction?
Stop taking the new medication and contact your pharmacist or doctor immediately. Don’t wait to see if it gets better. Document what you took, when, and what symptoms you’re having. If you have severe symptoms like chest pain, trouble breathing, sudden weakness, or uncontrolled bleeding, go to the ER. Bring your complete medication list with you. Early intervention can prevent serious harm.




13 Comments
Write a comment